Managing Complex
and Pathological Wounds
with Integra®
A Gallery of Cases
Marc E. Gottlieb, MD, FACS
Arimedica
version, 2005.
Limited
portions originally published as:
Gottlieb
ME. Management of
Complex and pathological Wounds with Integra. In: Lee BY, ed. The Wound Management
Manual. New York, McGraw-Hill,
2004: 226-289. (ISBN
0-07-143203-5).
Arimedica
version, expanded, with mostly new content and case studies, 2005.
Copyright
© 2004, 2005, Marc E. Gottlieb, MD
Content
may be used for non-commercial educational purposes.
Content
may not be republished, nor used for commercial purposes without prior license
or permission, except as permitted as “fair use” under United States copyright
laws.
Contacts:
Marc E. Gottlieb, MD, FACS
Plastic Surgeon,
Phone: 602-252-3354
Fax: 602-254-7891
Email: megott@arimedica.com
INDEX OF CASES
Case study A1, indications and surgical planning
Case study A2, indications and surgical planning
Case study A3, indications and surgical planning
Case study A4, indications and surgical planning
Case study A5, indications and surgical planning
Case study B1, acute care and critical coverage
Case study B2, acute care and critical coverage
Case study B3, acute care and critical coverage
Case study C1, reconstruction
Case study C2, reconstruction
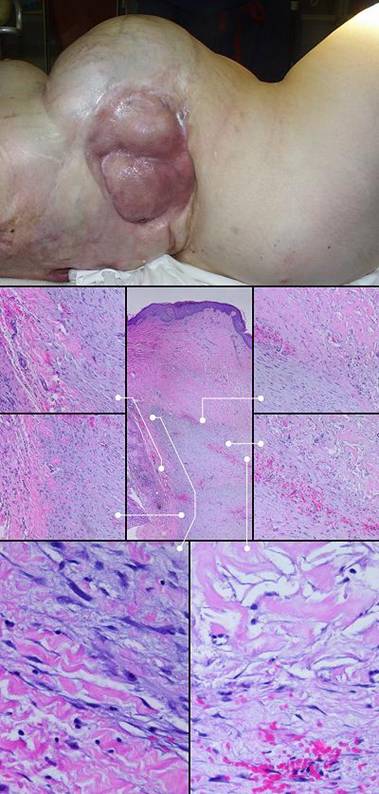
Case study C3, reconstruction, keloid
Case study D1, outcome type 1a, nominal reconstruction, healed
Case study D2, outcome type 1a, nominal reconstruction, healed
Case study D3, outcome type 1b, healed after ancillary care
Case study D4, outcome type 1d, healed after second Integra
Case study D5, outcome type 2a, partial success, healed after secondary flap
Case study D6, outcome type 2c, persistent open Integra
Case study D7, outcome type 3c, failure, amputation
Case study E1, diagnosis, venous
Case study E2, diagnosis, immunopathic
Case study E3, diagnosis, immunopathic
Case study E4, diagnosis, hypercoagulable
Case study E5, diagnosis, hypercoagulable
Case study E6, diagnosis, arterial disease
Case study E7, diagnosis, arterial disease
Case study E8, diagnosis, arterial disease and diabetes
Case study E9, diagnosis, diabetes, necrobiosis
Case study E10, diagnosis, granulomatous
Case study E11, diagnosis, atypical infection
Case study E12, diagnosis, mechanical
Case study E13, diagnosis, metabolic
Case study F1, location, upper extremity
Case study F2, location, trunk
Case study F3, location, leg
Case study F4, location, foot
Case study G1, exposed structure, bone
Case study G2, exposed structure, joint
Case study G3, exposed structure, hardware
Case study G4, exposed structure, lung
Case study H1, select problem, achilles
Case study H2, select problem, heel
Case study H3, select problem, stump salvage
Case study H4, select problem, dorsum of hand
Case study I1, performance, resistance to recurrence
Case study I2, performance, tumor
Case study I3, adjunct use, flap delay and donor site
Case study I4, technique and management, complete excision
Case study I5, technique and management, redo Integra
Case study I6, technique and management, planned second Integra
Case study I7, technique and management, not using Integra
Case study I8, technique and management, tissue engineering
PART 1
Integra and Chronic Wounds, Comparison to
Conventional Methods and Surgical Planning
Case studies A1 – A5
Integra does not replace conventional methods of wound surgery. All methods are important, and reconstructive plastic surgery and wound surgery are, at their core, a doctor’s “black bag” of principles and techniques which are selected and applied based on individual circumstances. When conventional repair, grafts, and flaps are likely to give the fastest, surest, most dependable, least complicated or disabling way to resolve a problem, that is what should be done. Since the majority of all surgery is done in people in whom physiological wound repair is intrinsically healthy, conventional methods will always be the most common. However, Integra is an important new tool in that black bag, because it can simplify care, make it safer, and succeed where conventional modalities fail. This is especially true in problem wounds where normal wound healing is damaged or inhibited. The best way to appreciate circumstances in which Integra is superior to conventional surgery for chronic wounds is to look at some case studies.
Case study A1, indications and surgical planning
73 year old man; embolic foot necrosis; leg salvage with Integra. The patient had embolization and distal foot necrosis following femoral catheterization for coronary angioplasty. Amputation through the distal tarsal row removed all necrosis. This is a functionally good amputation because all major ankle stabilizers, including tibialis anterior and peroneus longus are still inserted. The dilemma is that there is insufficient skin to close the wound (figure 17a). If more bone is removed for the sake of skin closure, the tendons will be disinserted, ankle control lost, and a below knee amputation would be warranted. There are no local flaps to cover the defect. Skin grafts are contraindicated over the open joints. The patient has atherosclerotic arteries making a free flap risky. Most surgeons would have opted below knee amputation. By placing Integra over the open osteotomies, these problems evaporate. Integra keeps the wound safe, tolerates arterial insufficiency, heals over bone, and bridges the joints. Skin grafts were placed at 6 weeks. They were completely healed and mature several months later. The patient wears a customized shoe and is fully ambulatory (figures 17b-e). Key points: Integra works where other surgical options will not; limbs can be salvaged; it is effective for arterial problems; it heals bones and joints; it avoids donor sites and additional complications in high risk wounds and patients.
|
Figure 17 Case
study A1
|
(a, top left) Amputation through the distal tarsus. Cuboid
and cuneiform osteotomies and intertarsal joints are open without sufficient
skin to close them. (b, top middle) Some of the lateral skin could be sutured without
tension, and everything else was covered with Integra, shown here stapled in
place before fixation dressings. (c, top right) The regenerated Integra a few days after placing
skin grafts. (d, bottom left) The healed result. Note that the Integra area
is smaller than it was originally. This diminution in size, with
corresponding dilation or advancement of adjacent normal skin is an
occasional occurrence. Representing normal accommodation to mechanical
load and anatomical geometry, all skin can do this, typically seen in the
atrophy of bulky flaps and surgical “dog ears”. It is different than scar
contracture because it remains compliant, not stiff, no tendinous banding,
without limitations of motion. (e, bottom right) At 5 months, the patient is walking normally in a custom fitted shoe. |
Case study A2, indications and surgical planning
74 year old woman; mixed pathological ulceration into the ankle; closed with Integra. The patient presented with a 30 year history of recurrent ankle ulcers, old skin grafts, and a nominal history of venous disease. Figure 18a demonstrates the frequent inflammatory papules and ulcers. Absence of venous stigmata such as edema, liposclerosis, and pigment changes, pertinent features such as history, distribution, and appearance of the lesions, and her ultimate response to antimetabolic chemotherapy confirm this as an immunopathy. The patient was already being treated with anticoagulants for a thrombotic history. Seronegative rheumatoid arthritis, Sweet’s neutrophilic dermatitis, and an antiphospholipid antibody syndrome are the most probable diagnoses. The lesions as seen were intermittently controlled with various treatments, but during an intense flare-up, all of the old skin grafts lysed. Ulceration was into the major underlying tendons and into the ankle mortise. The author treated this by excision and closure with a scapular free flap. At 9 and 10 days after surgery, gastrointestinal bleeding forced discontinuation of anticoagulants. The flap promptly began dying from its margins inward (the vascular anastomoses were patent at the time of debridement 4 days later, a characteristic history with hypercoagulable disorders). The ankle now requires closure. Further free flaps are contraindicated. Local flaps are not large enough, and they risk necrosis because of disease. Skin grafts cannot cover the open tendons and joint. Amputation would be considered by many surgeons. Interim biological dressings are suitable, but the closure dilemma cannot be avoided indefinitely. This was the author’s third Integra case. Integra was not used in the anticipation that it would work. It was used as a temporization, a biological dressing to buy time while alternate options were considered. It healed, and stayed healed through 4 years of follow-up (figure 18b). It was one of the seminal cases that led to this chapter. Similar cases would now be managed preemptively with Integra rather than by any other method. Key points: closure of essential structures; resistant to underlying pathology; succeeds where other options have failed; durable long lasting result resistant to future ulceration.
|
|
Figure 18 Case study A2 (a, top) A view of the chronic lateral ankle
pathology. Acute and chronic inflammation of decades
duration are affecting old skin grafts. A few months later, intense
inflammation lysed all of the skin in this area, leading to the failed free
flap and then Integra. (b, bottom) Integra was placed over the fibula, the open ankle
joint just anterior to the fibula, and the surrounding soft tissues.
The image shown is two years later. The Integra has been problem free,
and inflammation and ulceration no longer affect the area. |
Case study A3, indications and surgical planning
44 year old woman; hypercoagulable disorder and chronic achilles ulceration; healed with Integra. The patient had a spontaneous achilles tendon rupture. Tendon repair was followed by multiple complications and necrosis of the tendon. The ankle was ultimately closed with a rectus abdominis muscle free flap and skin grafts. The patient presented to the author for consultation because of villous dysplasia of the skin grafts, chronic recurring ulceration, and pain and dysfunction (figure 19a). The plan was to do serial excisions of excess old flap and advancement of surrounding skin. The first such procedure caused prompt dehiscence and necrosis of the wound. These events and a history of retinal artery thrombosis pinpoint a hypercoagulable disorder, confirmed by multiple post-acute elevations of fibrinogen and anticardiolipins. Any further effort to close and revise this wound has these challenges and requirements: any incision risks more necrosis and complications, a free flap already failed to give a desirable result and more donor sites are unwarranted, more skin grafts will have the same problem of mechanical dystrophy and ulceration, the reconstruction must be mechanically compliant and thin enough to accommodate normal footwear. Wound debridement and warfarin anticoagulation were followed by Integra. There were no further adverse events. A second piece of Integra was placed after the first one regenerated, in order to get a thicker neodermis in this area of significant stress and strain (figure 19b). The area healed without any of the pathological changes that affected the original skin grafts. (figure 19c). Key points: works well for hypercoagulable disorders; prevents pathergy; behaves like normal skin in areas where biomechanical loads adversely influence scars and skin grafts.
|
(a, left) Skin grafts over muscle flap over missing achilles
tendon. Villous dysplasia of skin grafts is common in areas of
repetitive mechanical strain, and the scar remains juvenile, hyperemic, pathologically active. There are multiple skin
ulcers near the distal end. |
Figure 19 Case study A3 (b, center) Integra in place. It is fully regenerated and
silicone is separating. It is desirable to place grafts before this
happens, but this does happen and is manageable as discussed in the text. (c, right) The reconstruction at one year. In contrast to what had happened with the original ordinary skin grafts, notice how this skin is thin, soft, compliant, with normal texture, that it has even developed the normal transverse dermal creases that occur in this area. |
Case study A4, indications and surgical planning
58 year old man; vascular infarction of hand; preservation of length with Integra. The problem resulted from accidental brachial artery drug injection (figure 20a). Initial debridement preserved metacarpophalangeal joints and proximal phalangeal bone, intending to use them as grafts under a hypogastric flap that would preserve some length and mobility. An abdominal pedicle transfer is an inherently difficult reconstruction, made more difficult here because of prior above knee amputation, an obese abdominal panniculus, cardiovascular disease, and depression. The patient opted out of this flap after 1 week, and all non-viable bone and joint was removed, just below the metacarpal heads. The margins of skin viability were a centimeter or two proximal to the osteotomies, creating a problem for closure. One option is to shorten bone, leaving him without metacarpals, but a mobile carpus. Aside from the general disabilities that this causes, it takes away this patient’s ability to hold a cane, crutch, or walker that he needs because of the ipsilateral thigh amputation. To preserve length, soft tissues are needed. A flap from the trunk was already a failed bad idea. A radial forearm flap is disqualified by the vascular injection injury, and so is a free flap. Skin grafts will either not take on the open bone, or will be prone to recurrent ulceration. The solution was to create a first web space by wrap-around of a dorsal skin flap over the thumb metacarpal, then closure of all wounds and osteotomies with Integra (figure 20b). After it was healed, tendon transfers and osteotomies in select areas were able to restore some mobility and pinch (figures 20b, c). In the author’s practice, Integra would now be opted as primary reconstruction for any such situation, abandoning the radial forearm flap and other traditional options just listed. Key points: preserves parts, length, and function; closes bone; works where other options are disqualified; no donor sites needed; no late revisions needed.
|
(d, bottom right) In this image at one year, the reconstruction is
matured. Skin is durable. Tendon and muscle transfers have
restored some flexion and pinch at the thumb base. The skin is healed
and trouble free, and the hand is functional for the
patient. |
Figure 20 Case study A4 (a, top left) The infarcted hand, prior to debridements.
Various ischemic areas can be coaxed to survive with good wound care,
pharmacological intervention, and patience. (b, top right) There is more salvageable hand than might at first
be appreciated. The problem is that there is not enough soft tissue to
cover remaining viable bone. Osteotomies are proximal to the metacarpal
heads. The first web space has been reconstructed with a dorsal skin
flap. Integra covers the bones and parts of the web space, shown at two
weeks. (c, bottom left) The healed hand. Some minor injury caused
abrasion at the end of the long finger, but that healed quickly. Thumb
carpometacarpal extension is preserved. |
Case study A5, indications and surgical planning
60 year old man; severe arterial disease with heel necrosis; leg salvage with Integra. The patient has diabetes, end stage renal disease, and severe atherosclerosis. Left foot ulceration resulted in septic gangrene, necessitating below knee amputation. While recuperating, he was allowed to get a large heel pressure ulcer. Toes on the right foot are already missing from previous vascular events. The patient was sent for consultation after refusing right leg amputation. The problem is how to close the large heel wound and preserve function. Severe arterial disease and deficient local resources preclude any type of local or free flap. Skin grafts are sure to fail over a calcaneal osteotomy accompanied by advanced vasculopathy. Integra easily solves the problem. It succeeds without donor sites nor other risk to the patient. It was managed as an outpatient, and the patient has maintained function and lifestyle (figure 21). Key points: same as for case A1.
|
(a, left) This is face on view of the reconstruction, healed
Integra over a large posterior calcanectomy and achilles insertion. |
Figure 21 Case study A5 (b, top center) The patient is in full weight bearing on his healed
foot. The oblique calcanectomy merely followed the contours of skin
necrosis; the toes are missing from previous
vascular complications. (c, bottom center) For stability, the patient uses a space filling orthotic wrapped around his ankle. (d, right) Using his sneaker, his left leg prosthesis, and a
walker, he is independent and ambulatory. |
PART 2
The author’s experience with Integra, at the writing of this chapter, is approximately 300 patients, far too many to present individually. The following examples have not been selected simply because they are “the best”, and many instructive cases with good outcomes and “bragging rights” are not presented. These cases have been selected exclusively on the basis of (1) being able to illustrate as many as practical of the specific points made in the text, (2) illustrating a wide enough spectrum of situations to permit a comprehensive understanding of when to use Integra, how to, and when not to, and (3) a suitable, even if incomplete, set of photographs exists. They are however typical and representative of the entire experience with Integra. The cases are grouped by subject. Each case is assigned to a particular category to draw attention to specific issues, but all cases overlap into different categories, and key points are listed for each case. The emphasis is on chronic wounds. In the D cases, “outcome type” refers to the outcome definitions in the “Review of Experience” section of the original chapter.
Acute Care and Critical Coverage
Case studies B1 – B3
Case study B1, acute care and critical coverage
7 year old girl, figure 22. Vehicular trauma caused complex degloving of the lower extremity, multiple skeletal injuries, skin and muscle avulsion, and injury to femoral and popliteal vessels. The foot was uninjured. Sciatic and tibial nerves, while neuropraxic, were anticipated to recover. Multiple staged procedures were required for wound stabilization and ultimate reconstruction. Instrumental was Integra’s ability to cover muscles, fractures, vessels, and other structures when other resources were limited. The patient is healed, foot sensate and normal, knee mobile without contractures, posture and ambulation normal. The only long term management is for femoral length discrepancy due to injury through the distal physis. Three years after injury, the patient participates in all manner of athletics and recreation without inhibition or significant limitations. Key points: protection of underlying structures; good mechanics and esthetics compared to skin grafts; useful where flaps are limited or destroyed; obviate free flaps; salvage limbs that might be amputated by most surgeons.
|
|
Figure 22 Case
study B1 (a, top)
The original injury, including distal femur fracture, knee injury, and
extensive soft tissue trauma. (b, bottom, left) A view of the patient a year and a half after injury.
Extensive soft tissue loss means that contours are not normal, but function
and lifestyle are. (c, bottom right) Close up view of the knee, flexed over the edge of a
table. Integra reconstructed skin, wrapped around the knee, is
compliant, having the full extensible range of motion needed for knee
flexion. |
Case study B2, acute care and critical coverage
37 year old man, figure 23. Group A streptococcal fasciitis developed after arthroscopy for a knee injury. The illustrations show just a fraction of the extensive debridement and drainage. Streptococcal toxic shock resulted in severe bone marrow depression with severe thrombocytopenia and a white blood cell count of only 200 / mm3. This, resulted in unrelieved wound derived septic shock in spite of aggressive antimicrobial therapies and liberal use of silver sulfadiazine. When the wounds were deemed ready for closure, Integra was used. Within an hour of closure, all pressor drugs could be discontinued, and the patient rapidly recovered. The patient has never required a follow-up procedure for the sake of correcting scar contractures. Key points: ability to immediately close a wound and control bioburden; ability to avoid graft donor sites in a patient who already has a wound greater than normal body surface area; ability to avoid additional trauma in the face of large fluid fluxes and hemodynamic instability; ability to avoid donor sites when anemia and thrombocytopenia create risks; ability to greatly simplify nursing care; good biomechanical results obviate late reconstruction for contractures; ability to save a life.
|
Figure 23 Case
study B2
|
(a, top left; b, top right) The right flank and thigh are shown several days
after debridement of acute streptococcal necrotizing fasciitis. There
are mirror image wounds on the left side, and similar involvement of legs and
chest. These are the wounds just prior to Integra. (c, middle left)
This is the right thigh just after placement of Integra. (d, middle right) This is the
same view six days later. Wrinkles in the material are due to a diminishing
wound area as muscle edema resolves. These “edema reduction wrinkles”
are common and of no consequence to usage and outcome. They do illuminate
Integra’s potent ability to control wound conditions, correcting inflammation
and its consequences. This permits rapid physiological recovery of the
wound, and it also causes prompt general improvements in critically ill
patients, sometimes profound. (e, bottom left; f, bottom right) The same views 5 months later. There are no
contractures, and late reconstruction is not needed.
|
Case study B3, acute care and critical coverage
32 year old man, figure 24. The patient has Milroy’s praecox primary lymphedema. Massive enlargement of lower extremities resulted in a sedentary existence without employment. Fasciectomy and skin reconstruction was performed, one side and then the other. This was an elective reconstruction which would have been essentially impossible without Integra. Integra permitted immediate closure of a very large wound, and avoided skin graft donor sites which would have doubled the wound area. The conventional approaches to this problem, fasciectomy with skin grafts or fasciectomy with preservation of local skin flaps, are notoriously complicated and have awful results. By handling the acute coverage and the reconstructive aspects equally well, Integra not only permits this type of reconstruction, but it gets good results. Lymphedema has not affected the reconstructed skin. The patient is now gainfully employed. Key points: ability to do extensive elective surgery with little risk; absence of donor sites simplifies care; good results for a problem that traditionally has only poor results with surgery.
|
|
Figure 24 Case study B3 (a, left top) The patient’s lymphedematous lower extremities are
shown prior to any surgery. Weight, volume, and dermatitis all
contributed to severe disabilities. (b, left middle) Four months after skin grafts. A few small
open areas require continuing care near mechanically active areas at the
knees. The patient is able to easily lift his extremity against
gravity, something not possible in many years. (c, lower) One year after
starting care, the grafts are healed. Note that the reconstruction has
not been affected by edema (diligent compression wrapping has also been
maintained). (d, right) The patient walks and has a job.
|
Reconstruction
Case studies C1 – C3
Case study C1, reconstruction
48 year old man, figure 25. The patient is a garden worker who lacerated his arm in a freshly manured yard, resulting in clostridial myofasciitis (gas gangrene). Drainage and debridement were followed by a period of topical care until the wounds met criteria for closure. Customary care for the open wounds of the arm and dorsal forearm would have been split thickness skin grafts, but Integra was used instead to avoid joint contractures and tendon and muscle tethering. This is a characteristic property of Integra, that applied directly to bare muscle, a shear accommodating areolar plane develops, permitting normal individualized muscle motion without any tethering to the skin. The patient rapidly regained full active range of motion, without needing any later surgery. This was preemptive reconstruction, fixing the problem before letting it occur. Key points: controls scar; prevents contracted joints; prevents scar tethering to muscles; prevents problems that would require late reconstruction; primary burn or trauma repair with Integra rather than secondary late reconstruction is more efficient and easier on the patients.
|
|
Figure 25 Case study C1 (a, top; b, bottom) Just a few months after having gas gangrene of the right upper extremity, the patient has recovered normal range of motion, shown here as full elbow extension and full wrist flexion and extension. Little formal hand therapy was needed. Integra can be seen on the distal arm at the elbow and on the dorsal forearm. |
Case study C2, reconstruction
11 year old girl, figure 26. The patient had severe dorsal wrist and elbow contractures from burn scars several years old. The old scars and skin grafts were excised, range of motion was restored by joint manipulation, and skin was reconstructed with Integra. The contractures were completely relieved, allowing normal range of motion with completely compliant skin. Key points: controls scar; reconstructs contracted joints; even if burn and trauma repair are not initially managed to prevent them, contractures can still be effectively relieved at any future time.
|
Figure 26 Case study C2 (a, b, c, left side) Volar (hand to the left), radial, and dorsal views
of the patient’s right upper extremity. Prior to this, the involved
areas were severely contracted, with distortion of fingers, wrist, and
elbow. Integra covers the antecubital fossa, a position guaranteed to
re-contracture if split thickness skin grafts only had been used. The
regenerated Integra is ready for skin grafts. (d, e, f, right side) Four months after Integra , there is no evidence of scar hypertrophy, skin distortion, nor joint contractures. The patient has 100% total motion of wrist and elbow. |
Case study C3, reconstruction, keloid
61 year old woman, figure 27. The patient developed typical ear keloids due to piercings. The patient is somewhat older than usual for the development of keloids, but recent attempts to excise it have resulted in recurrence. Excision and closure with Integra resolved the problem. Key points: controls scar; effective for keloids, contractures, and scar hypertrophy.
|
|
Figure 27 Case study C3 (a, left) Posterior view of the right ear showing a typical
recurrent keloid. (b, right) Same view a few months after keloid excision and closure with Integra. There is not the least evidence of any scar hypertrophy. |
Outcome Type
Case studies D1 – D7
Case study D1, outcome type 1a, nominal reconstruction, healed
51 year old woman, figure 28. The patient is a dialysis dependent diabetic with tertiary hyperparathyroidism. Multifocal ulceration developed due to systemic calcinosis-calciphylaxis. She had typical debilitating pain. The condition is refractory to usual topical and surgical care, with progressive necrosis being common. All necrotic areas were excised and closed with Integra. Pain and progressive ulceration immediately ceased. All areas healed quickly. This is the paradigm Integra reconstruction, complete success without delays. Key points: control of pathergy; permits safe debridement and wound closure without progression of necrosis; ability to heal problems usually considered recalcitrant; avoids high risks that would accompany conventional procedures.
|
|
Figure 28 Case study D1 (a, left) This is the histopathology of hyperparathyroid
calcinosis and ulceration, medial arteriosclerosis of small blood vessels,
some thrombosed. (b, c, top) The patient had numerous infarcted lesions on the
trunk. The right breast and right flank (lower abdomen) are shown
here. (d, e, bottom) The healed lesions 3 months after excision and Integra. |
Case study D2, outcome type 1a, nominal reconstruction, healed
70 year old man, figure 29. This patient had a chronic ankle ulcer due to post-phlebitic venous reflux and hypertension. Difficulty maintaining a healed wound in spite of good care prompted excision. Integra was opted for closure because of the mechanical risks across the ankle and at the malleolus. This was another nominal reconstruction, promptly healed. Key points: dependable use for venous problems; succeeds in mechanically active areas; durable result not prone to reulceration.
|
|
Figure 29 Case study D2 (a, left top) This venous lesion has been repetitively healed and
reulcerated, and it is now refractory to topical care. (b, left bottom) This is the excisional defect. The ankle
joint, malleolus, related ligaments, and motion make skin graft take and
durability somewhat uncertain. Integra was used to ensure a durable
result. (c, right top) The healed ulcer 7 months after excision. (d, right bottom) One year later, the Integra has remained
healthy. This image was taken as acute venous dermatitis caused new
ulceration on the medial malleolus, but this old area was unaffected by
nearby inflammatory changes.
|
Case study D3, outcome type 1b, healed after ancillary care
69 year old woman, figure 30. The patient had a prosthetic knee arthroplasty for complications of advanced rheumatoid arthritis. Peculiar ulceration developed near the ankle following surgery. It failed to improve with topical care and anti-inflammatory therapy. Laboratory diagnosis revealed Factor V Leiden heterozygous, low proteins C and S, and high homocysteine. Arterial ankle-brachial index was 0.93, and periwound transcutaneous oxygen pressures were 4 – 50, increasing to 200 – 330 breathing 100% O2. These studies confirm a hypercoagulable disorder without arterial macrovascular disease. Warfarin was started. The wound was excised and reconstructed with Integra (hyperbaric oxygen might have been a worthwhile adjuvant, but the patient was intolerant of it; see discussion under “Technique and Management – ancillary therapies” section). Excision and Integra immediately improved the patient, but complete epithelialization after skin overgrafts was slow. After 2 months of incomplete progress, platelet derived growth factor was used to accelerate epithelial growth and force closure. This patient showcases many of the properties and virtues of Integra, as further explained in the figure legend. Key points: control of inflammation and pathological wound behavior; coverage of essential structures; succeeds in a high risk patient; elimination of donor site risks; resistant to recurrent disease; complete epithelialization with PDGF; role as an artificial skin; symptomatic relief.
|
|
Figure 30 Case study D3 (a, top left) The original left lateral ankle ulcer. Note
periwound inflammation and lytic necrosis of the margins, typical of
rheumatoid panniculitis and hypercoagulable disorders. (b, top right) After 6 weeks of general wound care, conditions are
slightly better, but inflammation persists and the wound is not
healing. Surgery is therefore indicated. (c, 2nd left) The excised wound, with exposed muscles, ligaments,
and tendons. Integra is warranted because skin grafts are unlikely to
take, both for reasons of disease and for essential coverage. The
excised wound is enlarged because of extensive calcinosis cutis which had to
be removed (visible in background, another pathological factor which would
have guaranteed failure of topical care and grafts alone). (d, 2nd right) Integra in place. Note how all vestiges of
inflammation have completely disappeared. |
|
(e, 3rd left) At two months after skin grafting, the original
graft has left multiple islands of epidermis, but epithelial growth is
retarded. Platelet derived growth factor was initiated. Note that
even though the entire reconstruction is not yet concluded, that the
regenerated Integra has created healthy tissue, that periwound inflammation
remains completely controlled, that there is no further
necrosis-lysis-ulceration. (f, 3rd right) The response to topical cytokine was accelerated
epithelial growth. (g, bottom left) The wound at 7 months after placing the skin
grafts. (h, bottom right) The patient had a serious flare of disease 6 months
later with multiple new ulcers on both legs. The original
reconstruction was spared. New Integra can be seen in the background
over the contralateral achilles. The patient died from that rheumatoid
flare, but the new Integra still served a purpose, as artificial skin, for
high grade control of pain, and obviating the need for regular dressings or
other attention to the problem. |
|
Case study D4, outcome type 1d, healed after second Integra
71 year old woman, figure 31. The patient had 30 years chronic ulceration of the distal half of the leg due to rheumatoid arthritis. Fasciectomy and Integra closed nearly the entire leg. However, a few small areas remained open, and they did not heal after a few months of topical care. Because Integra was inherently successful, these small areas were covered with new Integra, and the leg was then completely healed. Key points: succeeds where all else has failed; use secondary small procedures when needed to complete a successful Integra reconstruction.
|
|
Figure 31 Case study D4 (a, b, top) Close up views of the chronic pathological rheumatoid
ulcers that encompassed the entire distal half of the leg. (c, 2nd row) After the first set of Integra, nearly the entire
leg is healed, but the few open areas shown would not close after several
months of topical care. (d, 3rd row) Four months after the second Integra, the leg is
healed. Anterior view. (e, 4th row) Lateral view. (f, bottom) Medial view. The small second pieces of
Integra already look quite mature and normal, but they stand out against the
first set of Integra which now is almost indistinguishable from nearby normal
skin. |
Case study D5, outcome type 2a, partial success, healed after secondary flap
86 year old woman, figure 32. The patient had chronic ankle ulceration of several years duration, probably venous. Anatomical structures were exposed, major tendons and the ankle joint itself. Excision and Integra healed the wound except for a small area due to shearing from the tibialis posterior tendon. A small local flap was used to cover this area, completing the reconstruction. Key points: closure of complex defects; use secondary small procedures when needed to complete a successful Integra reconstruction; no risk or significant donor sites in a high risk patient.
|
|
Figure 32 Case
study D5 (a, top) Integra
in place on the medial right ankle after ulcer excision. Note that this
is a large ulcer, and coverage is over ankle joint and multiple tendons and
ligaments. (b, middle)
The wound is nearly healed. The unepithelialized flat surfaces would have
healed by themselves with a few more weeks of topical care, but exposure and
shearing of the tibialis posterior tendon requires explicit closure.
Small blue dots demonstrate the length of excursion of the tendon. (c, bottom) A small flap from the dorsum of the foot closed the
tibialis tendon. Note how the Integra reconstructed areas are no
different than normal skin, soft, compliant, wrinkling and folding in
response to ankle motion. Normal dermal mechanics were already evident
in figure b, even before the entire area was healed. |
Case study D6, outcome type 2c, persistent open Integra
75 year old man, figure 33. The patient has extensive chronic venous disease and ulceration unresponsive to all treatments over many years. Excision and Integra healed most of the wounds. However, due to special circumstances, the patient had to plan months in advance for surgery, and then he had to return quickly to his usual work. He was unable to comply with all details of prescribed care, and some small areas that should have healed have not. His care has capitulated to a program of long term maintenance for the remaining open areas. While this cannot be considered an ideal result, to the patient it is quite acceptable. Compared to what he had, these residual wounds are much smaller than before Integra, drainage is less, pain is gone, and he remains functional. Key points: effective results even when not fully healed; patients are more accepting of big improvements than their doctors are of less-than-perfect results.
|
|
Figure 33 Case study D6 (a, top) Medial right leg. Long standing venous
hypertension and chronic stasis dermatitis have caused pronounced
dermatosclerosis and ulceration. There are similar ulcers laterally and
on the left leg. (b, middle) Skin, fascias, and wounds were excised, veins
stripped, and skin reconstructed with Integra. Shortly after skin
grafting, the Integra is healthy. The bare areas where skin grafts did
not take completely are otherwise healing properly, and complete
reepithelialization is expected. (c, bottom) As the reconstruction neared completion, consistent
good care could no longer be enforced. Several small ulcers persist,
and even the Integra reconstructed skin has developed venous pigmentation,
shown here one year later. While not fully healed, chronic
inflammation, pain, drainage, and other symptoms are well controlled, so the
current situation has been an improvement. |
Case study D7, outcome type 3c, failure, amputation
52 year old man, figure 34. The patient is an insulin dependent diabetic with advanced neuropathy, already black-balled by other physicians as non-compliant. He was referred for a last chance attempt to salvage a complex plantar wound. The foot was closed with Integra and local flaps. Integra intrinsically performed well, in large part because of special compliance enforcing orthotics that kept the patient off of his foot. As the skin grafts healed, the splints were removed, and without picking up his prescribed custom footwear, the patient promptly took a long motor vacation out of state. The resulting injury to the reconstruction was managed by below knee amputation. Key points: any effective care can be subverted by a non-compliant patient; diabetic plantar neuropathic ulceration is a relative contraindication for Integra.
|
Figure 34 Case study D7
|
|
(a, top left) The patient has already had posterior
calcanectomy. This image is looking into the subtalar joint. The
rest of the foot shows typical neuropathic and Charcot changes. (b, top right) In surgery, the wound has been excised and
partially closed by a plantar flap. Integra will be placed over the
wound seen here, including tendons, bone, and common plantar vessels. (c, bottom left) Skin grafts have been placed on regenerated
Integra. They are growing to confluence and keratinizing, on their way
to a technically good result. (d, bottom right) Integra and grafts are healed and healthy in peripheral areas. In the center, denudement of epithelium, callus at the margins, and pressure necrosis in the center all attest to weight bearing and ambulation without wearing proper footwear and orthotics. |
Diagnosis and Underlying Disorders
Case studies E1 – E13
Case study E1, diagnosis, venous
77 year
old man, figure 35. The patient has long standing refractory venous
ulceration. The usual order of management is good topical care and
compression, followed by venous interruption, and then excision and skin grafts
if needed. Most venous ulcers will heal within that traditional scope of
care. An obvious reason for using Integra instead of customary one stage
skin grafts is to cover essential structures (cases D2 and D5). Another
reason to use Integra is the one that applied here, multiple failed prior skin
grafts. After the usual period of good wound preparation, Integra healing
was prompt and uncomplicated, with long term durability of the
reconstruction. Key points: Integra succeeds when other
reasonable care has failed; Integra reconstruction for venous disease is
dependable.
|
|
Figure 35 Case study E1 (a, top left) Venous ulcer of right medial ankle, appearance upon
presentation. There is extensive dermatitis, and a necrotic piece of a
recent skin graft is still attached. (b, bottom left) After two weeks of basic hygiene, topical steroids,
and compression, acute conditions are controlled. Integra was opted for
closure for two reasons. One was the history of multiple failed
grafts. The other was the anticipation that, after years of
inflammation and ulceration, underlying anatomy would be exposed after
excision, and that local biomechanics would require better coverage than an
ordinary skin graft. |
|
(c, top right) Excision leaves behind the exposed posterior tibial
neurovascular bundle and an open achilles fat space. (d, bottom right) In conjunction with continued elastic compression,
everything remains healed and healthy at one year. |
|
Case study E2, diagnosis, immunopathic
77 year old man, figure 36. This patient with long standing rheumatoid arthritis developed an ankle ulcer. It did not improve with customary topical care. Integra was opted because of the failure to respond to care (indicative of persistent soft tissue pathology), and proximity of the ulcer to the ankle and achilles where motion is apt to create problems. In a healthy patient, skin grafts or dependable local flaps (such as a “reverse sural nerve flap”) would have been the simplest and quickest thing to do, but challenged by active rheumatoid, Integra was the safest thing to do. Integra healed quickly. Key points: low risks in a high risk patient; essential closure of achilles tendon.
|
Figure 36 Case
study E2
|
|
(a, left) Right
posterolateral heel ulceration in a patient with rheumatoid arthritis.
It is a typical rheumatoid lesion, characterized by multifocal lysis of skin
and fascias. (b, middle)
After a month of basic care, including intralesional steroids, the wound is
not improved. There is some control and wound healing in a few areas,
but there is also persistent inflammation and marginal necrosis.
Spontaneous improvement is not expected. (c, right) Several months after Integra, the area is
healed. In this image, the patient has some contact dermatitis due to
continued use of dressing materials even after everything else healed.
This eczematous reaction cleared promptly with some topical steroids.
The Integra reconstructed skin is inherently healthy, looking quite normal at
the periphery of the dermatitis, but this demonstrates that Integra skin can
also be affected by injury and injudicious care. |
Case study E3, diagnosis, immunopathic
41 year old woman, figure 37. This patient had characteristic multifocal rheumatoid ulceration along synovium and tendons of both feet and ankles. Topical care failed, and multiple skin grafts dissolved. Integra induced immediate and complete cessation of inflammation and ulceration for each and every wound. Multiple tendons and interphalangeal joints were covered and healed. However, the first set of skin grafts had only limited take. After a couple of weeks of hygienic topical care, the healthy open Integra was regrafted. The patient had a strong family history of early cardiovascular death, and shortly after the second skin graft, she died from thrombosis of her coronary artery stent. While the final result was not achieved, this case does highlight important aspects of Integra. Key points: potent ability to control soft tissue pathology; superior control of immunopathic ulcers; improved quality of life through control of symptoms and simplified care; good performance even when it is bare of an epithelial cover.
|
|
Figure 37 Case study E3 (a, left top) The medial left ankle. In spite of some
nominal recent care and failed skin grafts, this is an active ulcerating
rheumatoid lesion, with lytic dissolution of skin and fascias. (b, left middle) The dorsum of the right foot with other necrotic and
lytic lesions. There were many other concurrent ulcers of both feet and
ankles, all located over tendon sheaths and joints, a typical lower extremity
manifestation of rheumatoid synovitis. (c, left bottom) All lesions were excised and closed with Integra,
the dorsum of the left foot shown here. The material is covering extensor
tendons and open toe joints. Inflammation and necrosis in the periwound
soft tissues have ceased. |
|
(d, right top) The initial skin grafts had limited take.
Images d, e, and f are concurrent, at the time of second skin grafting.
They show healthy happy regenerated Integra. The original wounds,
sequestered under the neodermis, are themselves closed and no longer
wounds. Only the Integra itself remains open, behaving as “naked” but
otherwise normal dermis. (e, right middle) Same as d. Epithelial ingrowth is evident at
margins, and some of the small wounds on the dorsum of the foot have
completely reepithelialized. All pre-Integra inflammation and necrosis
are completely gone. These images demonstrate Integra’s ability to
control pathergy, local soft tissue pathology, chaotic wound dynamics, and
persistent inflammation and necrosis. While healed skin grafts are the
goal, open regenerated Integra is always healthier than the original
wound. (f, right bottom) Similar findings on the left foot. This is now
a healthy non-pathological wound. Integra successfully closed the open
tendons and joints. Although the patient died before the reconstruction
was complete, she had several weeks of pain free healthy wounds. |
|
Case study E4, diagnosis, hypercoagulable
61 year old woman, figure 4. Hypercoagulable ulceration. See figure 4 legend for more details. Also notable is that the fibula immediately underneath the ulcer had a large dysplastic osteophyte. This is because chronic ulceration over bone often causes hyperplastic new bone due to the effects of transforming or pro-proliferative growth factors which are perpetually in the wound. Tangential tibial ostectomy was done to get smooth wound surfaces, and Integra was applied to the osteotomy. Key points: control of periwound inflammation; prevention of pathergy; success when other treatments have failed; ability to close bone.
|
|
Figure 4 Case study E4. This 61 year old woman had leg ulceration and
failed care for many years, along with a history of multiple venous
thrombosis and pulmonary embolism. Note that the usual stigmata of
venous disease, pigment, edema, dermatosclerosis, are not very severe.
This is a hypercoagulable ulcer rather than a common post-phlebitic venous
problem, confirmed by histology (microthrombi; long
standing warfarin therapy precluded making the exact pre-thrombotic
diagnosis). |
|
|
(4a,
top left) The ulcer prior to
aggressive consistent topical care. (4b, top right) After stricter care and increased warfarin, the wound
and periwound are improved, but nevertheless, inflammation and active
necrosis-ulceration persist at the margins. (4c, bottom left) Six days after wound excision and Integra,
periwound inflammation, erythema, and edema, have
completely subsided. (4d, bottom right) Healed. As the first case cited in the text, this
is a good example of a chronic refractory ulcer due to active pathology which
failed multiple prior care but healed promptly with Integra. |
|
|
Case study E5, diagnosis, hypercoagulable
45 year old woman, figure 38. The patient was seen in consultation after multiple amputations for multifocal necrosis and ulceration. Skin infarction and progressive limb loss were active and ongoing, exacerbated with each amputation and debridement. The patient did not have atherosclerosis. Laboratory workup showed high homocysteine levels. Warfarin anticoagulation and hyperbaric oxygen therapy were started. Thigh and hand wounds were excised and closed with Integra, arresting all further necrosis. The patient has been healed and problem free for 4 years. Key points: control of pathergy; permits safe debridement and wound closure without progression of necrosis; eminently suited to hypercoagulable ulcers and necrosis; indiscriminate progressive amputation is avoidable with thoughtful diagnosis and effective treatment; saves lives and limbs.
|
|
Figure 38 Case study E5 (a, top) Prior to Integra, the patient was critically ill,
with active progressive skin necrosis. The patient had already had bilateral
above knee amputations, and higher amputations and
death were threatened. Necrosis was arrested and the wounds were all
healed after proper diagnosis and effective treatments were started
(anticoagulants, hyperbaric oxygen, Integra). In this view, healed
Integra is seen on the lateral and posterior thigh. (b, c, bottom) Necrosis was multifocal, including some small hand
lesions. Integra is shown here over a finger lesion that ulcerated into
the distal interphalangeal joint. In these two views, the healed lesion
is shown at rest and with the long finger flexed, demonstrating good
compliance in the graft. |
Case study E6, diagnosis, arterial disease
64 year old man, figure 39. The patient has aortoiliac atherosclerosis. Toe necrosis resulted in progressive levels of amputation, each complicated by further necrosis. The patient was referred when thigh wound necrosis left few other options. Oxygen tensions in the thigh were very low, but large vessel revascularization was not possible. The necrosis was excised, covered with Integra, and the patient had adjunct hyperbaric oxygen therapy. Healed. Key points: control of vascular pathergy; no risk due to incisions or donor sites in a high risk wound or patient; a good treatment choice when there are no conventional good choices.
|
Figure 39 Case study E6
(a, left) This recent thigh amputation has been complicated by
skin and fat necrosis. While many surgeons regard above knee
amputations as usually safe, they are not when there is aorto-iliac
occlusion. This is an instructive case study about the challenges of
doing wound and soft tissue surgery in the presence of arterial
insufficiency, where the principles of good care create their own problems
and compete with each other. One of the surest ways to kill ischemic
tissues is to subject them to any kind of tension. Tension creates
pressure which can exceed blood pressure in an underperfused part. That
means that suturing an ischemic wound will kill it, and leaving the wound open
and unstressed is therefore preferable. However, another ischemic flap
killer is an open wound. Regardless that an open wound is safe and
healthy and a mandatory necessity of effective care of soft tissue pathology,
highly ischemic tissues can be intolerant of exposure. Desiccation,
bioburden, inflammation, and injurious topical medicaments will all cause
progressive infarction. This thigh is the perfect example of this
clinical perplexity. Do an amputation and sew it up,
and it dies. Leave it open, and it dies.
Damned if you do, damned if you don’t. This wound was sutured, and the
adjacent tissues died. Had it been left open, or if the wound is now
debrided, it will likewise develop superficial necrosis, comparable to case
study F4 (figure 50). Integra solves this dilemma, because you can
debride the wound and then immediately close it without stress or tension on
the tissues. By arresting inflammation, it controls yet another factor
which threatens the ischemic wound. (b, middle) In this image two weeks after debridement and
Integra, the wound is healthy, and there is no necrosis at any of the
margins. (c, right) Healed after skin grafts. |
Case study E7, diagnosis, arterial disease
67 year old woman, figure 40. The patient developed foot necrosis due to complications of atherosclerosis. Arterial revascularization was performed. The foot was debrided and closed with Integra. Healed. Key points: averts threatened amputation; heals over bones and joints; revascularization (or correction of any underlying disease) should always be done when possible; no donor or incision risks in a high risk extremity.
|
|
Figure 40 Case study E7 (a, top left) Extensive arterial necrosis of this foot was managed
initially by basic topical are and debridement, along with operative
revascularization. Saphenous vein bypass to the dorsalis pedis artery
has been done, and the wound has responded with rapid proliferation of
granulation tissue. Prior to revascularization, the foot and a potential
below knee amputation had the same risks and dilemmas as case E6. After
successful revascularization, the issues become much simpler, only a matter
of good wound preparation, then essential closure in a locale where no flaps
are available. (b, top right) The wound was debrided and closed with Integra,
shown here 6 weeks after placement and ready for skin grafts. |
|
(c, bottom left) The healed foot 6 months later. (d, bottom right) An inferior view showing the healed reconstruction
over the plantar calcaneus and over a posterior calcaneal osteotomy.
The patient uses custom footwear for control of pressure and shear in these
areas. |
|
Case study E8, diagnosis, arterial disease and diabetes
74 year old man, figure 41. The patient has diabetes and atherosclerosis leading to forefoot amputation. This case is very similar to case A1, and the same general commentary applies. The biggest difference is that case A1 was one of the earlier cases in the author’s experience, and using Integra to salvage an open transtarsal amputation was done with some uncertainty about the outcome. This case was done without a moment’s thought to any option other than Integra. There should no longer be any need to throw away a perfectly good extremity only for the want of a good flap. Integra ought to be seen as the preferred option for salvaging complex foot wounds in high risk patients. Two years later, this patient remains completely ambulatory and active. Key points: closes complex wounds with open bone and joints; prevents higher level amputations; preserves quality of life; manageable strictly as an outpatient; very effective for arteriopathic and diabetic patients.
|
Figure 41 Case study E8
(a, top left) The open foot after transtarsal amputation.
The cuneiforms and intertarsal joints are exposed and require cover. (b, top middle) The amputation closed with Integra. It is
stained red from bleeding at the time of surgery, but this is of no
consequence. (c, bottom left) The healed foot. (d, bottom middle) Lateral view of the foot demonstrating active
dorsiflexion through the tibialis anterior tendon, confirming that major
tendons remain inserted and active. (e, right) Using an insert at the front of a regular
shoe, and a thin ankle-foot orthosis for some additional stability, the
patient remains very active, leading a normal life. |
Case study E9, diagnosis, diabetes, necrobiosis
53 year old woman, figure 42. This patient has longstanding diabetes. Vascular complications have not occurred, but necrobiosis lipoidica of the legs has accompanied the disease since early adulthood. Persistent painful inflammation and ulceration, unresponsive to any prior therapy, have caused chronic illness and social anxieties. The problem has been cured by complete excision of diseased and ulcerated fascias followed by Integra reconstruction of the skin. Malaise and fatigue have resolved due to elimination of chronic inflammation, and she no longer feels compelled to hide her legs. Key points: maintains control of local pathology; acceptable esthetic results; succeeds where all else has failed; makes a difference in people’s lives.
|
|
Figure 42 Case study E9 (a, top) Necrobiosis lipoidica diabeticorum. A view of
the right leg prior to surgery. Chronic inflammation, necrosis,
ulceration, and fibrosis are advanced. (b, middle) The leg after excision and placement of
Integra. Lesions on the left leg were also excised and covered. (c, bottom) Skin grafts were placed at six weeks. This
image is 9 weeks after the grafts. The last few small open areas are
nearly healed, and the patient is otherwise completely healthy. Note
the dermal wrinkling orthogonal to underlying muscle fibers over the anterior
and lateral compartments, a sign of maturation and normal mechanical skin
compliance (compare this to the thick scar present in the same locations
prior to excision and reconstruction). |
Case study E10, diagnosis, granulomatous
55 year old woman, figure 43. The patient had many years of leg ulceration refractory to care. Many prior skin grafts failed. When seen in consultation, diagnostic workup could not identify a particular cause. Complete wound excision was performed, for debridement and diagnosis, in anticipation of new skin grafts to be placed within a few days. However, within days of excision, the wound had indurated margins and peculiar proteinaceous plaques indicative of active pathology. Histology showed granulomatous inflammation, but atypical pathogens could not be recovered. While Integra was not originally planned, it was now chosen because of its ability to control persistent or chaotic wound pathology. While not necessarily expected to work, it did, and the healed wound has remained stable for several years. Key points: succeeds where all else has failed; controls non-specific or chaotic soft tissue pathology.
|
|
Figure 43 Case study E10 (a, top) The nearly circumferential leg wound is shown days
after excision. Granulation tissue is indicative of an inherently healthy
wound repair process. However, note the waxy white plaques, persistent
edema at the ankle, and the thickened wound margins at the inferior
edge. These findings are indicative of some type of active unresolved
pathology. (b, middle) Integra in place, fully
regenerated and ready for skin grafts. There is neither edema nor any
other sign of inflammation or disease. (c, bottom) In this view, there is a small area posteriorly
which is a little red and immature. This is where the skin overgrafts
did not take and required some extra topical care. However, there is no
evidence of active disease. At 8 months, everything is healed, the
first time in many years, free of inflammation and ulceration. |
Case study E11, diagnosis, atypical infection
58 year old woman, figure 44. With a long history of rheumatoid arthritis and treatment, this patient developed progressive leg ulceration and critical illness. Aspergillus was diagnosed histologically. Complete fasciectomy and Integra closure was performed (amputation also would have been appropriate but was refused). The patient rapidly stabilized, with improvements in general metabolic, hemodynamic, and ventilatory parameters. However, she then developed complete renal failure from (encapsulated) amphotericin B. The family also refused dialysis, and the patient died from uremia. The acute physiological corrections were comparable to cases B2 and H4. Had the patient survived, the anatomical outcomes would have been comparable to cases D4, F3, and G1. While there are no final pictures to show, this case illustrates how Integra can be used in the management of atypical infections. The principles are the same as for any mycotic or mycobacterial abscess: total excision and antimicrobial drugs, and then wound closure. Integra should be used for large anatomically complex wounds and for fragile patients. Key points: rapid stabilization of wounds and general physiology; no donor sites nor additional operative risk in an unstable patient.
|
|
Figure 44 Case study E11 (a, top) The left leg, with aspergillus fasciitis. (b, middle) The debrided leg. As with many conditions
portrayed in these case studies, this disease affects skin and subcutaneous
fascias, but spares the “working parts”, neurovascular and musculoskeletal
structures. Absent arterial insufficiency, these are all manageable
problems. Extremities need not be amputated simply because skin is
missing. (c, bottom) One week later, the Integra is in place and
healthy. Note the wrinkles in the material, due to reduction of leg
volume and surface area as inflammation and edema subside, reflecting the
physiological improvements that occur when Integra closes a wound. |
Case study E12, diagnosis, mechanical
79 year old woman, figure 45. The patient has a chronic ankle ulcer of many years duration, unresponsive to any prior treatment. Workup failed to reveal any diagnosis other than chronic pseudarthrosis at an old malleolar fracture directly underlying the ulcer. Excision of the ulcer, bone fragments, and arthrosis was closed with Integra. The significance of tissue mechanics and their influence on mesenchymal differentiation and repair is overlooked by most physicians. The cardinal signs of pseudarthrosis are inflammation and pain, and in a susceptible elderly person, it can create enough local pathology to maintain an active ulcer. Healed. Key points: control of chaotic wound dynamics; effective over bone and joint.
|
Figure 45 Case
study E12
(a, left) This
right lateral malleolar ulcer has been present several years, refractory to
all prior care. Note the intense eczematoid dermatitis surrounding the
ulcer. A malleolar fragment and pseudarthrosis are
underneath. (b, middle)
The wound was excised, and Integra has been placed over bone and joint and
ligaments. Note that inflammation has completely subsided. (c, right) The healed wound. |
Case study E13, diagnosis, metabolic
46 year old woman, figure 46. The patient has pannicular calcinosis (calcifying panniculitis). Calcium is precipitated extensively throughout subcutaneous fascias. Involvement in this case is circumferentially around the pelvis, over both hips, and down both thighs laterally to the knees, with patchy calcinosis of other thigh surfaces. This is a characteristic but advanced distribution of an uncommon disorder. Like all calcium dystrophies, this problem can be a primary diagnosis in an otherwise healthy patient, or it can be associated with a variety of disorders. In this case the patient has dermatomyositis, and chronic cutaneous and pannicular inflammation may have been etiological. Her disease is now controlled by methotrexate, and she is free of other acute illness. The calcium tumor over the left hip became ulcerated and abscessed, a problem which has no solution other than excision. Dense confluent rock hard calcinosis means that excision is all-or-none. Note that this is not a case of Integra-or-nothing. Conventional skin grafts would have been a perfectly suitable alternative, but the advantages of Integra are two. First, it simplifies care, by closing the wound immediately, avoiding secondary wounds created by skin graft donor sites, and thereby controlling drainage, pain, and short term disability. Second, long term results are apt to be better. In this case, just as in case B3, extensive resection of skin and fascias was done electively, without donor sites. All care was outpatient. Contractures have not occurred, and no type of late revision will be needed. At one year, there is no disease in the reconstructed hip and thigh. Key points: permits aggressive elective resection and reconstruction; keeps complex care manageable as an outpatient; obviates need for late reconstruction; resistance to disease; results in happy healed patients.
|
Figure 46 Case study E13
(a, left) The left hip and thigh at the time of
resection. Hyperpigmented areas along the thigh and lumbar indicate the
location of calcinosis. Over the hip, numerous sinuses are draining the
abscess within the calcium tumor. (b, center) One year after excision and Integra, the area is
healed. There has been no recurrence of pathology. The patient’s
general welfare is greatly improved by elimination of chronic infection.
This photograph was taken just prior to the same procedure on the right
side. Calcinosis is equally extensive on the right, but because it is
not yet abscessed, there has been no urgency to operate. The fact that
the patient returns to have the other side operated is a testimonial to
patients’ acceptance of these procedures: good results, control of disease,
and a return to healthy lifestyle, with acceptable post-operative discomfort
and little risk or time away from home. (c, right top) These two pictures illustrate some options for graft
fixation. In this image, the right side has been excised and closed, as
an outpatient, 4 days prior. The pelvis is a challenging area to use
wrap-on bandages, so the Integra was compressed and immobilized with a
“tie-over” type of dressing using an elastic bandage zigzagged and stapled
over bulk cotton gauze. (d, right bottom) The stapled dressings are very effective
compression, but they can be untidy and uncomfortable. They were used
of necessity in the operating room, but 4 days later in outpatient clinic,
they were replaced with a sponge vacuum device (V.A.C.®,
Vacuum Assisted Closure ™, Kinetic Concepts, Inc., |
Location and Anatomical Area
Case studies F1 – F4
Case study F1, location, upper extremity
42 year old woman, figure 47. The patient has diabetic atherosclerosis involving the upper extremities. Long finger ulceration resulted in progressive necrosis and amputation. At the time of consultation, there was abscess and necrosis of the central hand. Debridement and silver sulfadiazine stabilized the wound, permitting the third ray defect to heal by natural contraction. However, exposed joints and flexor tendons required coverage to avoid ring finger amputation. Vascular disease and loss of the adjacent finger precluded any of the customary flaps that ordinarily solve this problem. Integra over the exposed structures of the ring finger succeeded, followed by a small flap to close residual open ligaments of the interphalangeal joint. Key points: low risk in a high risk situation; suitable when customary options do not exist; simplicity, low risk, and good results make it a preferable choice even if customary options are available; effective for vascular problems; essential closure of important structures.
|
|
Figure 47 Case study F1 (a, top) This left hand presented with active progressive
infarction and abscess beginning in the long finger ray. This image is
after a few weeks of good wound hygiene, silver sulfadiazine, and
debridement. Arterial pressure and circulation are not as bad as first
thought, evidenced by the completely healed central hand. Since
initiating good topical care, gross inflammation (erythema, edema, and so on)
are controlled, and there has been no further necrosis. The hand is
healing, but essential coverage issues over the skeletal structures of the
ring finger need a solution. The usual flaps from adjacent fingers
cannot be done in this high risk arteriopathic hand. (b, middle) The prepared wound ready for Integra. Crucial
structures to be covered are the web space, the proximal interphalangeal
joint, and the flexor tendons and their sheath. (c, bottom) The healed hand. The interphalangeal joint
had a persistent small ulcer after Integra, and this was closed with a small
flap from the dorsum of the joint. Integra closed the flexor tendons, and it reconstructed a fully compliant web space
free of scar and contracture. Interphalangeal joint motion is limited,
but the patient eschewed therapy and is very happy to have a healed hand
without having lost the ring finger.
|
Case study F2, location, trunk
49 year old man, figure 48. This paraplegic patient had chronic lumbar ulceration due to vertebral osteomyelitis and extensive bone abscess at the site of his original lumbar injury and surgery. Complete three level vertebrectomy, L2 - L3 - L4, was required to cure the problem. Repair had to satisfy closure of remaining bone, dura, and spinal cord, protection of intraabdominal vascular structures just anterior, and sufficient mechanical stability to prevent subsidiary ulceration or excessive disability. The most crucial structures were closed with available flaps of lumbar muscles, fascias, and skin. Integra was a complement to the flaps, closing all other open surfaces, providing essential coverage and simplifying post operative care. The patient has been healed and functional for two years, using a spinal orthosis for stability in his wheelchair. Key points: simplifies care in an unusual situation; works well in combination with flaps, each contributing what it does best for the reconstruction.
|
|
Figure 48 Case study F2 (a, left top) A view from caudad to cephalad showing the lumbar
area after 3 level total vertebrectomy. Available skin and paraspinal
muscles have been elevated or transposed to close key structures. (b, left bottom) The wound closed with flaps and Integra. (c, right) The patient is healed and independent, seen here a year and a half later. By wearing a TLSO (thoraco-lumbo-sacral orthosis), the patient is stable and mobile for transfers and wheelchair activities. |
Case study F3, location, leg
77 year old woman, figure 49. The patient had bilateral leg and ankle ulceration for 40 years. In spite of classic symptoms of Sjögren’s disease, the diagnosis was missed countless times. When seen in consultation, the diagnosis was made, anti-inflammatory and antimetabolic treatments were started, and the patient’s general health status improved considerably. Fasciectomy and Integra reconstruction healed the legs. Key points: succeeds where all else has failed; succeeds when patients and providers think the situation is hopeless; especially helpful for treating extensive ulceration due to connective tissue disorders.
|
|
Figure 49 Case study F3 (a, left top and middle) The
patient has extensive bilateral “rheumatoid” ulceration of 40 years duration
due to Sjögren’s disease. (There are three sets of images,
before-during-after. There are 4 views for each time. The image
order is matched, beginning from the top: medial right leg and ankle, lateral
left, medial left, lateral right.) |
|
(b, center top and middle) The legs and ankles one week after excision and
Integra. The material covers multiple muscles, tendons, and retinacular
ligaments. Notice the wrinkling in the Integra, a common occurrence
because inflammation is controlled and all edema is gone, decreasing the
circumference of the extremity. (c, right column) The healed legs two years later. An anterior
view is also shown. (d, bottom row) Close up views of the medial and lateral right ankle, to show the quality and texture of the regenerated skin. |
|
Case study F4, location, foot
73 year old man, figure 50. The patient required transmetatarsal amputation for atherosclerotic necrosis of the toes. The open incision, well cared for, was not an immediate threat to the patient, but it would not heal, and slow progressive necrosis continued on the wound surface. Hyperbaric oxygen therapy was offered but refused because the patient lives and works at a far distance. The wound was excised and closed with Integra, and the patient continued his normal activities. Integra stabilized the wound. It remained healthy after silicone removal (unlike the open wound’s behavior prior to Integra). Slow epithelialization was accelerated with platelet derived growth factor. Healed. Key points: control of pathergy; succeeds where most surgeons would have done a leg amputation; good topical wound care, hygiene, and patience give much better results than amputations due to impatience; PDGF is a useful adjunct; function, lifestyle, and vocational productivity can be preserved, even during reconstruction; all outpatient care.
|
|
Figure 50 Case study
F4 (a, top left) The
left foot many weeks after transmetatarsal amputation. The wound is
rigorously cared for, and it has remained free of inflammation and
complications. However, the foot remains severely ischemic, and there
is the perpetual accumulation of superficial necrosis in spite of regular
debridement. (b, top right) Closure
with Integra arrests necrosis. The foot is fully motored and
functional. (c, bottom left) Open Integra, two months after regeneration and silicone
removal. Skin grafts did not adhere, and the wound is not
epithelializing. However, although epidermis is not moving, the
regenerated Integra is acting like “naked dermis”, healthy, protecting the
wound, preventing necrosis. In the interest of stimulating epithelial
growth, platelet derived growth factor is now being used topically. (d, bottom right) Healed and ambulatory 3 months later. |
Exposed Structures
Case studies G1 – G4
Case study G1, exposed structure, bone
33 year old man, figure 51. The patient has had multiple venous thrombosis and leg ulceration ever since a femur fracture at age 14 (while not worked up for such, laboratory evaluation of recent similar patients has demonstrated that young men with a comparable history almost uniformly have Factor V Leiden or similar pre-thrombotic disorder). Under the author’s care, a large ulcer healed, but in spite of continuing compression and preventive care, it recurred a year or two later, and surgery was opted. All inflamed, ulcerated, and trophic skin was excised. The tibia, highly dysplastic due to chronic contiguous inflammation, was planed down to remaining normal cortex, and the wound was closed with Integra. The wound has been healed and stable nearly 5 years. Key points: durable reconstruction that outlasts other approaches to care; closes bone; no donor sites nor other risks as would be the case with free flaps; outpatient care.
|
|
Figure 51 Case study G1 (a, top) The right leg in surgery. Pathological tissues
have been excised. Dysplastic tibial cortex is exposed. (b, middle) After planing the tibia back to architecturally
normal bone, the wound is ready for closure with Integra. (c, bottom) At 5 months, the reconstruction is almost
completely healed (it has since healed and has remained stable for 5 years).
|
Case study G2, exposed structure, joint
43 year old man, figure 52. An internationally ranked athlete, this patient rapidly deteriorated due to scleroderma. He presented with multiple hand problems, including ulceration into the index finger metacarpophalangeal joint. As one of the few fingers not contracted and still otherwise functional, salvage was important for the most rudimentary activities of daily living. Any incisional surgery was risky because of immunopathy and related vascular problems. Even if surgery was safe, sclerotic skin made local flaps a technical impossibility. Integra healed the open bone and joint, with preservation of a functioning finger. Key points: works where anything else is too risky; no further incisions or risk; coverage of bone and joint.
|
|
Figure 52 Case study G2 (a, top left) The right hand in surgery. The open index
finger metacarpophalangeal joint and degenerated bone at
the base of the phalanx have been debrided. Various contracture
releases have been performed on other fingers. Note skin atrophy,
sclerosis, and telangiectasias typical of scleroderma. |
|
(b, top right) Histology of the debrided specimen shows stenotic
fibrotic arteries typical of immunopathic angiopathy. Impaired
circulation adds another layer of risk and complexity to this case. Of
the conventional options for closure, topical care, repair, flaps, grafts, or
amputation, all are either too risky, doomed to fail, technically unfeasible,
or too destructive of remaining function. There are no rational
solutions to close this wound, nothing safe, nothing
which will get a favorable result, other than Integra. (c, bottom left) The healed hand at 6 months. This is the
posture at rest. The healed Integra over the joint, soft and compliant,
has dermal creases. (d, bottom right) The material is compliant enough to allow full
flexion. Due to extensive fibrosis, failed prior operations, and lack
of systematic care, the hand prior to consultation was useless. After
this Integra reconstruction and related activities, socioeconomic factors
hampered his ability to have aggressive hand therapy and follow-up
reconstruction. While this result is only as good as circumstances
permitted, it has healed the hand and restored basic activities of daily
living. Daily care is no longer needed, pain and symptoms and threat to
the limb are gone, and he can now hold a pencil, telephone, cup, and
toothbrush. |
|
Case study G3, exposed structure, hardware
50 year old woman, figure 53. The patient had a distal tibia fracture treated by plate and screw fixation. Skin dehiscence was managed by rectus abdominis and latissimus free flaps, both of which died. When seen in consultation, the first jobs were to stop all other surgery, clean up the wound, and work her up for autoimmune and hematological disorders (a diagnosis was not established). Options for surgical closure of an open distal tibia are already quite limited, and in this case, all choices, local flaps and free flaps, carried substantial risk of further failure. Rather than take these risks, Integra was opted. Its intended use was to be a high grade artificial skin. Whenever silicone would threaten to come off, new Integra would be placed, and this would continue until the fracture was healed and the exposed plate could be removed, probably 3 or 4 months. It was not meant to completely close the wound over the plate, but because of tangential histoconduction, that is what happened. After the third piece of Integra, a complete competent lamina of new tissue covering the plate could be skin grafted. There were no complications nor setbacks of any kind. The patient became quite skilled with the required care, permitting her to take an out-of-country holiday vacation for three weeks while the third Integra was in place. It has remained healed for two years, the hardware uncomplicated and still in place. Key points: controls pathergy; safe; not susceptible to the pathological failures that normal repairs, flaps, and grafts are subject to; solves problems when other options have run out; tangential histoconduction; essential closure; role as a high quality artificial skin; multiple serial Integra is a good strategy, to be used for artificial skin purposes or for reconstruction; outpatient care.
|
|
Figure 53 Case study G3 (a, left top) The right distal tibia after two failed free
flaps. Note the multifocal infarction of skin edges, all suspicious for
vascular, hematological, or immunopathic disorders, even though an underlying
diagnosis was not established. The tibialis anterior tendon, the metal
plate and screws, and the fracture underneath are all exposed and need a
solution for coverage and salvage. After a period of hygienic wound
care, Integra was used to close this wound, according to the rationale
discussed in the text. (b, left middle) After a few weeks, Integra has fully opacified over
those surrounding soft tissues that could directly source regenerative cells
into the matrix. Integra sponge over plate and tendon has not yet
regenerated. Filled with yellow serum, the plate can still be seen
through it. Because silicone ejection was imminent, the original
silicone has been peeled off in surgery. Skin grafts will be placed on
peripheral regenerated areas, and new Integra will be placed over the central
zone. |
|
(c, left bottom) In this and image b, look closely at the margins of the central
sponge. In many areas, opacified new tissue is diffusing inward from
the surrounding normal areas. This centripetal growth will continue
until the entire matrix has generated tissue. (d, right top) While tangential histogenesis alone was not the
original surgical plan, it became obvious early in the process that it was
going to work. After the third Integra (and skin grafts), the leg is
healed. The leg is seen here 11 months after starting the
reconstruction, entirely healthy and uncomplicated (anterior view, foot to
the left). (e, right middle) The patient is fully ambulatory and active, with no
restrictions of activity of any kind. The fracture is healed, and the
plate and screws remain in place. Ankle dorsiflexion is off by 20
degrees, but this can be a consequence of fracture, and it is better than
having the whole foot off. (f, right bottom) Demonstrating plantar flexion, which is normal. |
|
Case study G4, exposed structure, lung
50 year old woman, figure 54. Advanced breast cancer caused abscess and necrosis of the upper extremity, with brachial plexus and chest wall infiltration. Radiation necrosis and ulceration of the sternum further complicated the problem. No distant metastasis could be identified, and the patient was recommended for interscapulothoracic amputation to relieve intolerable symptoms. Most forequarter amputations have normal thoracic skin that allows primary wound closure. The operation in this patient was undertaken knowing that if the resection was to be effective palliation, justifying the procedure at all, that all nearby skin, parts of the musculoskeletal chest wall, and all usual flaps would be gone. Without Integra there was no coverage, and surgery simply could not have been done and would not have been scheduled. Excising the chest wall without any flaps meant that Integra was used to cover open thorax and lung. The patient died 10 months later. Patient and family reported that the experience was worthwhile because pain and other symptoms were almost completely relieved, and travel and family activities were possible for a few months. The Integra was an effective skin and a competent chest wall, developing an alveolar fistula only in the last few days of life. Integra was also placed over known micrometastases, without visible growth of the tumor in those areas. Key points: effective over well debrided irradiated areas; role in palliative care; support of meaningful lifestyle; effective for chest wall and abdominal reconstruction; sometimes the only possible option; makes extreme surgery feasible and relatively easy; no donor sites when they can be ill afforded; a good companion to flaps (see figure legend); possible tumor control?
|
|
Figure 54 Case study G4 (a, top left) The chest, abdomen, and neck after wide resection
and interscapulothoracic amputation for widely infiltrated breast cancer.
The first rib and apical chest wall have been removed, and the lung is
exposed. The anterior chest and sternum are areas of radiation exposure and
superficial ulceration. Posteriorly,
the extent of resection is comparable, crossing the midline. The rectus
abdominis muscle is the only potential flap that might be used, but its
viability is uncertain when transposed to the base of the neck. There
are no options for closure other than Integra. Other than 10 days
associated with this first operation, the care was outpatient. |
|
(b, top middle) Two weeks after surgery, Integra was healthy except
anteriorly over the irradiated areas. A second procedure was done, anterior
debridement and new Integra, and also delay of a rectus flap. Integra was
serving as a very effective chest wall substitute, but there was uncertainty
about leaving it as the only long term coverage over the lung. So,
preparation of the rectus muscle was started so that it would be safe to pull
up this far. In this image 2 weeks later (4 weeks after the first
operation), the original Integra is fully regenerated. The new 2 week
Integra is healthy (except for the characteristic black color over two dead
ribs). The delay incisions are visible on the upper abdomen. (c, bottom left) Three weeks later, skin grafts are healing posterior
and lateral. The new anterior Integra is healing properly.
Degenerative exudates surround the two dead ribs, but this does not influence
the rest of the reconstruction. Regenerated Integra is still in place
over the lung. (d, bottom middle) It is now 3 months after the first operation.
Skin grafts are healing across the entire chest. The flap has been
transposed and covers the lung. A piece of Integra has been placed on
the bare undersurface of the flap, to keep it healthy and to obviate the need
for any specific care. This piece of Integra is regenerated, still
under silicone, an innocuous neodermis that obviates any direct care. (e, right top) These two images are at two weeks. The lung is
visible under the Integra which is just beginning to opacify. This
first image shows the lung in inspiration. There is the expected
paradoxical inversion of the material, but the lung stays suspended and
inflated, obviously without pneumothorax or effusion. (f, right 2nd) The companion image, during positive pressure
valsalva. (g, right 3rd) During the various procedures, the original Integra
over the lung was replaced with a second Integra when the first piece was
ready to lose it silicone. This image is at the time when the second
silicone was removed and the lung was covered with the rectus flap. The
lung is still visible through the thin but regenerated Integra,
and it remains fully inflated, even with the silicone peeled off. When
the patient later started chemotherapy, fat necrosis developed at the distal
end of the flap, exposing the Integra. Fortunately, the Integra
neodermis remained a competent chest wall for another 6 months. (h, right bottom) Several months later, cutaneous tumor metastases are
beginning to grow, visible in the lower left of this image. At the time
of initial surgery, histology had confirmed microscopic disease across the
chest wall, now under Integra. If it was going to grow, one might
expect it to be obvious through the thin Integra, just as ordinary skin
grafts in this situation rapidly become ulcerated by tumor growth.
However, except for a limited number of small nodules, the Integra was not
host to tumor growth, at least not obvious exophytic
growths nor malignant ulceration. In this image, there are a few
open areas of still healing skin graft, and a few nodules near the normal
skin, but little other sign of neoplastic tumor growth. |
|
Special Problems
Case studies H1 – H4
Case study H1, select problem, achilles
65 year old woman, figure 55. The patient has Wegener’s granulomatosis with severe pulmonary disease and an achilles ulcer. After a period of preparational wound care and treatment of disease, the ulcer and tendon were closed with Integra. The reconstruction healed promptly. Key points: essential closure; eliminates flaps in high risk wounds; safety in high risk patients, excellent results over the achilles tendon.
|
|
Figure 55 Case study H1 (a, top) A view of the ulcerated achilles tendon. There
are multiple scars from previous immunopathic or vasculitic ulcers.
Granulation tissue around the tendon indicates that wound healing is
intrinsically competent. However, disease is still active, and shearing
from achilles tendon motion means that this wound cannot easily heal, if at
all, even in a healthy person. (b, 2nd) In surgery, the wound has been prepared by
excisional debridement, including decortication of tendon until only healthy
fibers remain. Serious consideration was given to using a “reverse
sural nerve flap” (the design marked in blue ink), a usually dependable flap
for wounds in this area. However, skin grafts would have been needed at
the donor site, so the flap would not really have simplified the situation.
Given the high risks for this wound and patient, good sense prevailed, and
the simplest safest thing was done, Integra. (c, 3rd) The regenerated material ready for skin
grafts. (d, bottom) The healed result two months later. |
Case study H2, select problem, heel
84 year old woman, figure 56. The patient developed multiple foot ulcers related to diabetic vascular disease and disabling senile illnesses. Living in a rural area with an elderly husband, foot preservation was required so that she could stand and assist with wheelchair transfers. All ulcers were debrided and closed with Integra, including a large heel ulcer requiring posterior calcanectomy. Reconstruction was uncomplicated, and all wounds healed. Key points: effective closure of heel; effective closure of bone; salvage of limbs and preservation of lifestyle without risk.
|
|
Figure 56 Case study H2 (a, top) The right foot is seen after debridement and Integra
reconstruction of multiple wounds, including the achilles tendon and the heel
which are visible in this view. The extent of posterior calcanectomy
can be seen from the missing heel contour. (b, middle) A close up view of the heel showing stable
skin. (c, bottom) The same view, but with the foot in forced passive
dorsiflexion. The contours of the achilles tendon insertion on the
calcaneal margin are seen in relief as the thin, compliant, scarless new skin
moves and conforms to activity underneath. |
Case study H3, select problem, stump salvage
53 year old man, figure 57. The patient had a below knee amputation for complications of diabetic atherosclerosis. Although wound necrosis threatened above knee amputation, it was managed by debridement, good wound care, and then reclosure with Integra. The stump healed, permitting the patient to be rehabilitated with a preserved knee. Key points: salvages complicated stumps; prevents progressive amputation; effective in diabetic atherosclerotic patients; recently healed Integra can be injured and lacerated by accidental trauma (see figure legend).
|
|
Figure 57 Case study H3 (a, top left) This left leg has stump necrosis after below knee
amputation. Note the granulation tissue. This wound is
sufficiently vascularized, and it is competent to heal. Necrosis was a
consequence of avoidable technical factors. With patience, good wound
care, and suitable surgery, this should be easy to heal, without higher
amputation as had been suggested to the patient. (In all of these
images, the tibial tubercle is at the top of
the image, the knee superior to that by a few centimeters.) (b, top right) After a period of debridement and good daily care,
the wound now meets criteria for reclosure. Note the exposed necrotic
tibial surface which will need excision. (c, middle left) The prepared wound ready for closure, including
decorticated anterior tibia. There are no dependable options, no
available flaps, no realistic choices for closure
other than Integra. (d, middle right) Integra in place 5 weeks later, nearing complete
regeneration and ready for skin grafts. (e, bottom left) The healed reconstruction two months later. A
few subsidiary wounds around the knee are also healing (not treated with
Integra). Throughout the reconstruction, a rigid posterior platform
splint was used to maintain an extended knee yet permit care of the wounds
and the reconstruction. Knee posture is now normal, and the patient and
leg are preparing for prosthetic training. |
|
(f, bottom right) One month later, the patient fell. This caused
a tangential avulsion laceration of newly healed epidermis. This was
treated like any similar laceration without difficulty. This image is
included to demonstrate that Integra reconstructed skin, like any wound or
scar or skin graft, needs suitable time to fully mature and develop
sufficient strength to bear up to the requirements of daily life.
Appropriate caution and care should be taken for several months after
reconstruction. |
|
Case study H4, select problem, dorsum of hand
44 year old man, figure 58. The patient developed staphylococcal necrotizing fasciitis after leg surgery. Extensive involvement of lower extremities, trunk, and upper extremities required usual aggressive debridement followed by wound care and then closure and reconstruction. Integra was used to close many areas, including leg amputation, knee joint, shoulder joint, and many tendons and muscles. The case is presented to demonstrate the type of dorsal hand wound which is easily reconstructed with Integra. This is also an example of Integra as a biological dressing, as a bulk filler, and as a planned second use of Integra (see figure legend). All wounds and structures closed with Integra have remained healed and uncomplicated for 4 years. Key points: high grade artificial skin; good tool for managing critically ill patients with large wounds; a superior dorsal hand reconstruction compared to other methods; the spongy matrix alone can be used for volume filling; Integra should be a first choice for the dorsal hand and wrist.
|
Figure 58 Case study H4
|
|
(a, top left) A view of the left upper extremity after
staphylococcal necrotizing fasciitis. Multiple other areas of the body
were similarly involved. After a week of debridement and initial care,
the patient is now back in the operating room ready to start closing
wounds. Note the drain passing through the glenohumeral joint.
The shoulder was not ready for closure and was kept open for another week of
care. (b, top middle) This image is one week later. All wounds
closed by Integra or simple direct repair have contributed to a healthier
more stable patient with fewer nursing requirements. The shoulder
itself is now clean and ready for closure. (c, top right) The Integra over brachial muscles, seen in image b,
has been pulled off. It served a function as high quality interim
closure, but now it has been removed for the sake of an integrated repair of
the entire shoulder area. A small flap of axillary skin was available
for transposition, so it was used. As good as Integra does for
preserving normal skin mechanics, flaps are still better in many areas.
In an area like the axilla, notorious for scar contracture, the opportunity
to do a simple composite reconstruction with a handy flap should not be
missed. Except for the final overgrafts, these wounds healed without
further ado. (d, middle left) However, in some areas, Integra is superior to
conventional flaps, and the dorsum of the hand is one of those areas.
In this image, the open dorsal hand and its tendons have been covered with
Integra. (e, center) This and the next image show the hand a year and a
half later, at rest and in flexion. (f, middle right) The dorsal hand Integra is thin, compliant, and
extensible. Dermal creases are present. There are no restrictions
on range of motion. Tendons and joints glide independently of the new
skin. The results are comparable to full thickness skin grafts:
good texture and mechanics; no need for late revision. The differences
are important: Integra is more apt to take completely than the grafts;
the supply of full thickness grafts is limited, but Integra is
unlimited; losing some full thickness graft is a waste that cannot
necessarily be restored, but losing some Integra, while unlikely, can easily
be replaced with more Integra. Integra ought to be seen as the
preferred option for reconstructing skin on the dorsum of the hand. (g, bottom left) The bottom row illustrates Integra for volume
filling. The patient’s fasciitis began in the leg after below knee
amputation. The stump wound is now ready for closure, but the defect
extends into the tibial medulla. Soft tissue is required to fill this
(or risk abscess if it is covered without filling). However, there are
no good options for local flaps. (h, bottom middle) Integra sponge was packed into the endosteal cavity
and deeper soft tissues, and then a normal bilaminate piece was used to cover the entire wound. The Integra will
be replaced with tissue, and in the short term, it is a reservoir of
antibiotics that will resist any tendency to get a dead space abscess.
Its use is comparable to antibiotic-laden acrylic cement, which is usually
used for bone filling. However, the Integra matrix will simply become
part of the host and will not require exchange. (i, bottom right) The silicone remained in place without complication
until the wound was regenerated. The skin grafts healed and the stump
has remained uncomplicated for 4 years. |
Performance, Adjunct Usage, Technique
Case studies I1 – I8
Case study I1, performance, resistance to recurrence
71 year old woman, figure 59. The patient was treated for “venous ulcer” for several years, even though the ulcer had paradigm features of rheumatoid disease and the patient met multiple other diagnostic criteria. On consultation, the diagnosis was made and anti-immune treatment was started. The ulcer, including open fibula, was closed with Integra. Two years later, disease flare-up caused multiple new ulcers on both legs and ankles. The original reconstruction was spared new injury. The new lesions were closed with Integra after preliminary management showed that they were not likely to heal by topical care alone. Key points: accurate diagnosis important; treatment of underlying disease important; essential closure of muscles, tendons, bone; durable results resistant to disease flare-up.
|
(g, bottom left) Medial view. Because the new ulcers and
fascial necrosis did not improve by anti-rheumatoid control and topical care
alone, they were excised and closed with Integra, shown here one week after
placement. (h, bottom right) Medial view. All healed, seen here 9 months
later. |
Figure 59 Case study I1 (a, top left) The original ulcer on the lateral left leg and
ankle. Multifocal lytic ulceration, exposure but sparing of muscles and
tendons, distribution along tendon sheaths, and absence of venous pigment and
edema all peg this as a rheumatoid ulcer (or related immunopathy). (b, top right) Integra in place after excisional debridement and
initiation of anti-inflammatory and antimetabolic therapy. (c, 2nd left) The healed ankle 6 months later. This area has
remained healed ever since. (d, 2nd right) Two years later, the patient became very ill with a
disease flare-up. Rheumatoid dermatofasciitis and multifocal ulceration
occurred, seen here on the medial side of the left leg. (e, 3rd left) Anterior view. After 3 weeks of increased
anti-inflammatory therapy and care of the leg, some inflammation has
subsided, some persists, and there are numerous small ulcers. (f, 3rd right) This image is simultaneous to figure e.
Whatever else has happened nearby, the original lateral leg reconstruction
remains healthy. This is because Integra does not restore the adipose
fascias in which rheumatoid panniculitis typically occurs, but also possibly
because, as a more embryonic type of tissue, it might have some inherent
resistance to these diseases. |
Case study I2, performance, tumor
22 year old woman, figure 60. The patient has juvenile nodular fibromatosis and Gardener’s syndrome. Multiple previous tumors and surgery had created areas of unstable scar and skin graft on the right flank, all of which lysed and ulcerated when she developed an acute nephric abscess. The area was closed with Integra and it remained healed, another successful Integra result, another example of visceral coverage (kidney and colon). However, one year later, mesenteric tumor growth and a persistent calyceal fistula necessitated block resection of abdominal wall, kidney, and bowel. The old Integra came out with the kidney. This case is presented because the histology of the specimen suggests that Integra might be a barrier to the growth of invasive tumor. Key points: visceral coverage; possible tumor control?
|
|
Figure 60 Case study I2 (a, top) The patient’s back and right flank prior to tumor
resection (hip to the right, chest to the left). The large mass
protruding anteriorly is a large thoraco-abdominal and mesenteric fibrous
tumor which is to be removed. In the center is one-year old
Integra. The two lobules to which the Integra conforms are kidney and
tumor. The Integra is inherently healthy, not invaded by tumor.
The calyceal-nephrostomy fistula is at the medial margin ( (b, center) Wide microscopic view of part of the specimen.
The top pink zone is healthy Integra, covered by mature epidermis and
papillary dermis. At the left margin is some conventional scar (see
figure 16). At left bottom is kidney. The right and center bottom
is tumor, juvenile nodular fibromatosis. While not a true sarcoma, this
neoplastic process is invasive and recurrent. The blue-grey tumor is
separated from kidney by some normal pink collagenous fascia. (c, middle left) These two panels zoom in on tumor margin along the
perinephric fascia. There is diffuse infiltration of tumor into the
fascia. (d, middle right) These two panels zoom in on margins of the tumor
adjacent to Integra. The tumor does not appear to transgress or invade the
Integra. (e, bottom left) A close up of the fascia margin shows organized
columns of tumor infiltrating into normal tissue. (f, bottom right) A close up of the Integra margin. A few tumor
cells seem to be flirting with the idea of crossing the line, but there is no
organization between these cells, and no bulk transgression. |
Case study I3, adjunct use, flap delay and donor site
14 year old boy, figure 61. The patient had a back ulcer of several years duration following radiation for a spinal tumor. Closure was done using a large lumbar (non-irradiated) flap. The flap required several delays and intermediate transfers. Integra was an adjunct to care. It was not used as the primary closure, but instead, it was used to close flap donor sites and to line the undersurface of the flap during delay. This is an important concept in staged flaps. The idea of delay is to develop robust circulation in the flap through a small inflow pedicle. A flap is typically raised and then put back in place, waiting until later procedures to be moved. If an already dissected undersurface is allowed to heal and reconnect, that completely abrogates the delay. In this case, effective delay made for a safe flap, and when the flap was moved, the underlying Integra was ready for overgrafts. All components of the reconstruction healed without complication, and the problem was easily managed as an outpatient with little pain and no disability. Key points: works well in conjunction with flaps; excellent companion to large staged and pedicled flaps; simplifies post-operative pain, nursing, and recuperation.
|
|
Figure 61 Case study I3 (a, top left) The lumbar area is a watershed between large
vascularized muscles, and the choice of large dependable one stage flaps is
limited. Closure of the right paraspinal radiation ulcer is to be done
with a random flap transposed in stages from the non-irradiated left lumbar
area. This image shows the flap elevated and moved into place over the
excised ulcer. Scar and dystrophic skin inferior to the flap is part of
the radiation injury, and this is to be excised and closed with the back end of the flap after the forward part of
the flap heals. (b, top right) Integra has been used over exposed muscles at the
flap donor site. This was done, rather than skin grafts, to minimize
pain, drainage, and nursing requirements. Part of any good flap delay
is to keep the elevated pedicle from healing and revascularizing on its deep surface.
Integra can also be seen buried underneath the flap to prevent this. |
|
(c,
middle left) Images a and b were photographed from the right side (head to the
right). Images c, d, e, and f are from the left side (head to the
left). Fourteen days later, a delay was done. Because the flap is
healing and revascularizing at its distal end, the base has been divided so
as to force more robust vascularization at the front end. This will
permit the back half of the flap to be elevated and moved in another few weeks.
The Integra has normal two-week appearance, still a transparent window on
underlying structures, but just starting to opacify from histogenesis.
The buried Integra cannot be seen, but this is the moment of its most
important function, because if the flap were able to revascularize on its
deep surface, it would not develop enough circulation at the distal end to
support the entire thing. (d,
middle right) Three weeks
later, the delayed flap is healthy, uncomplicated, and ready for
transposition. The Integra is fully regenerated and ready for skin
grafts. (e,
bottom left) Taken at the
same time as image d, this is the back end of the flap, elevated and ready to
move. The underlying Integra is healthy, and it has done its job,
keeping the flap unconnected in that area, easy and bloodless to elevate,
without creating new vascular stresses on the flap. The tail of the
flap was moved across the midline to replace the remaining dystrophic
irradiated skin. Skin grafts were placed over both pieces of regenerated
Integra. (f, bottom right) A year later, everything is healed. The flap
is healthy, Integra regenerated skin is soft and compliant, and there has
been no skin dystrophy nor ulceration. |
|
Case study I4, technique and management, complete excision.
60 year old woman, figure 62. The patient had a persistent leg ulcer refractory to various care. Progressive lytic ulceration with spotty pigmentation suggested a venous, vasculitic, or other immunopathic disorder (but an exact diagnosis was not established). This profile prompted excision and Integra, and the ulcer healed. The case is presented to illustrate the method of ulcer excision and Integra placement. Key points: proper technique; good wound preparation; complete ulcer excision; proper graft fixation; continued care of the healed result; relatively resistant to disease, but not impervious to injury and neglected care (see figure legend).
|
|
Figure 62 Case study I4 (a, top left) The right leg ulcer. Spotty brown pigment
suggests venous insufficiency or hypertension. However, the ulcer
itself has features more typical of immunopathies and hematopathologies
rather than ordinary venous stasis ulceration. Various topical
treatments and compression failed. Anticipating that skin grafts would
not take, and that flaps might be subject to complications or impaired
healing, excision and Integra was elected. While disease is still
active, as evidenced by a retarded wound module and signs of active necrosis
and ulceration at the margins, nevertheless, this wound has been properly
prepared for surgery. Periwound erythema is mostly gone, there is
little or no edema, and the only residue on the surface is
from silver sulfadiazine cream. |
|
(b, top right) The excised wound. All of the original wound
surface must be removed. Note that the deep plane of resection
incorporates the deep or muscular fascia (the “sural fascia” here on the
leg). Since musculoskeletal and visceral structures are not usually
affected by these disorders, excision of susceptible tissues must be done
until these structures are revealed. This is a mandatory treatment
principle, and it explains why so many Integra cases have essential coverage
issues, and why Integra is so suitable for their closure. (Note that
the specimen remains attached by the superficial peroneal nerve. This
nerve perforates the sural fascia and terminates in its target territory in
this position. Almost all chronic wounds in this position are tethered
by this nerve, explaining why most anterolateral ulcers are predictably
painful.) (c, middle left) Integra has been placed on the wound and secured
(staples in this case, but choice of method is irrelevant). Excess
material at the margins is then trimmed. In spite of its collagen
content and microporous surface area, recall from figure 5 that Integra is not thrombogenic nor hemostatic. Wound bleeding
should be controlled before the material goes on. (d, middle right) Post-operative care is minimum or none, because the
reconstruction is protected under fixation or compression bandages.
They are usually changed once a week, but more often or less often depending
on circumstances. In this case, this is the first dressing change at 10
days. The Integra is healthy and normal looking for this interval,
without yet any histogenetic opacification. (e, bottom left) Six weeks later, the material is regenerated and
ready for skin grafts. (f, bottom right) The skin grafts did heal, but four months later,
the patient developed some superficial ulceration of the new epidermis.
This resulted from inconsistent use of prescribed compression garments and
skin care. Basic topical care and good compression corrected the
problem, and the wound quickly rehealed, shown here as epithelium has once
again grown to confluence. |
|
Case study I5, technique and management, redo Integra
90 year old woman, figure 63. The patient developed heel and achilles pressure ulcers while recuperating from a femur fracture. Operative debridement and closure with Integra was performed, including posterior calcanectomy for the large heel defect. It became obvious, from black discoloration of the Integra sponge, that there was still dead calcaneal bone that was not fully excised. The Integra was left in place as a temporary artificial skin. During the second procedure, skin grafts were placed over the regenerated achilles, and new Integra was placed on the heel after further ostectomy. Final skin grafts were placed a month later. The wounds healed, and the patient continued with rehabilitation. The results have remained stable for 2 years. Key points: effective simple closure of heel and achilles; effective artificial skin; sequential use of Integra in select circumstances; necessity of thorough excisional debridement prior to placement.
|
|
Figure 63 Case study I5 (a, top) Integra was placed on a calcaneal ostectomy and over
the achilles tendon. The first piece of heel Integra turned black due
to incompletely excised bone necrosis (the black color is characteristic of
Integra over non-viable tissues, such as in image b where it overlaps normal
keratinized skin, or in figure 54b). During the second procedure, skin grafts
were placed where ready, on the achilles, and a progressive calcaneal
ostectomy was covered with new Integra. In this view a week later,
achilles skin grafts and the new heel Integra are healthy . (b, 2nd) Three weeks later, the second heel Integra is
regenerating properly. (c, 3rd) Five months later, all is healed and healthy. (d, bottom) The following year, the reconstruction continues to
be healthy, without any injury or ulceration due to footwear, walking, nor
other normal activities. |
Case study I6, technique and management, planned second Integra
69 year old woman, figure 64. The patient had necrosis and ulceration of the leg following excision of a small benign skin lesion.. It failed to heal with customary care, and slow necrosis and ulceration continued. Foot pulses were good, and laboratory studies showed protein C deficiency and the presence of cryoglobulins. Warfarin was started, but anticoagulation and topical care alone still did not induce wound module healing. Conventional skin grafts and local flaps are contraindicated because they will have the same complications that caused the ulcer in the first place. Excision and closure with Integra controlled the wound and permitted healing. However, by the time that the first piece of Integra was regenerated and ready to loose its silicone, the flexor digitorum longus tendon was not yet covered. A second piece of Integra was applied over the entire reconstruction, and skin grafts could be placed after that. Key points: control of pathergy; ability to bridge structures; multiple sequential Integra buys time and allows the reconstruction to completely regenerate.
|
|
Figure 64 Case study I6 (a, top left) Right medial leg ulcer. Active necrosis and
ulceration at the margins are still active, even with good topical care,
edema control, and anticoagulation. (b, top right) In this histologic section, the ulcer surface is at
the top left corner. Inflammatory exudates are sparse, due to good
hygienic care and the fact that the cause of this was not an inflammatory
disorder. Subjacent blood vessels have stasis and thrombosis, and the
vessels themselves are necrotic, typical of microthrombotic disorders. (c, middle left) Integra in place. There has been no further necrosis nor ulceration. The flexor
digitorum longus tendon is visible underneath. |
|
(d, middle right) The silicone has been removed showing that the
Integra has regenerated everywhere except over the flexor digitorum
tendon. This is not a failure, but merely a need to apply a second
serial piece of Integra. (e, bottom left) After the second piece regenerated, skin grafts were
applied. Three months later, all is healed, and the double barrel
contours of the tibialis posterior muscle and the flexor digitorum tendon are
easily seen. (f, bottom right) Two years after that, the reconstruction remains
healthy. |
|
Case study I7, technique and management, not using Integra
77 year old man, figure 65. One case is selected to illustrate when not to use Integra. This patient with long standing rheumatoid arthritis had an ankle ulcer over the medial malleolus. Malleolar ulcers generally do not heal without surgery because of local mechanics, shearing due to foot motion, and wound geometry related to the malleolar bursa. This patient’s history sounds in principle like many of the other cases presented. However, there are important differences. His rheumatoid arthritis is not very active, and he is not ill. The ulcer is due to minor impact trauma in the presence of weakened senile skin, but there has been no dermatitis nor ulcerative inflammation. Although one might anticipate atherosclerosis due to his age, he in fact has normal pulses. This is a simple mechanical ulcer. Risk factors for failed surgery or impaired healing are more speculative than real. The ulcer and malleolar bursa were excised then closed with conventional flaps and grafts, concluded in one operation. Integra would have worked well, but it would have unnecessarily prolonged the care and required a second operation. The flap also gives a superior result, being more tolerant of future trauma (see case H3). Key points: choose the best option to get the best result efficiently and with minimum morbidity.
|
Figure 65 Case study I7
(a, left) Medial right ankle with malleolar ulcer. The
skin defect is deceptive, because there is a bursa underneath. The
malleolar bursa is normal anatomy. The bursa is there to accommodate
motion of skin over bone, and it extends another centimeter or two in most
directions. Once the skin perforates into the bursa, the mechanics of
the mesenchyme dictate that this cannot heal. A trial of topical care
is always appropriate (as was done), but it will quickly confirm that this
lesion requires surgery. (b, middle) The lesion has been excised. A small local
flap was transposed from the anterior ankle to close the bare debrided
malleolus. A full thickness skin graft taken from near the knee closed
the flap donor site. A customary “tie-over” dressing holds the graft in
place. (c, right) The reconstruction is healed. The thick flap
over the malleolus provides protection against future accidental injury. |
Case study I8, technique and management, tissue engineering
82 year old woman, figure 66. The patient had a skin cancer of the scalp treated by radiation, 6500 cGy, resulting in a chronic ulcerated parietal cranium. Compounding the problem was advanced Paget’s disease of bone with atrophic immobile skin making scalp flaps impossible. The calvarial wound was vascularized and viable, just not wound healing competent. Restoration of competent tissue with trapezius flaps or free flaps would have succeeded, but having had several failed operations, she refused any more major surgery. She did agree to minor outpatient procedures. The solution was to use Integra as a carrier of healthy cells. The reconstruction started by placing a small fenestrated plastic chamber under abdominal skin. Two weeks later, proliferative tissue within the chamber has removed. It was mashed, partly trypsinized, and filtered. The resulting paste was worked into a piece of Integra which was applied to the debrided scalp wound. The composite implant remained alive, the matrix serving as an incubator of mitosis-competent cells. There was a bloom of multifocal regenerative loci distinct from normal Integra regeneration patterns, indicating that the Integra was healing by the seeded cells. When the first piece regenerated, a second unseeded layer of Integra was placed to build a thicker lamina of new tissue. Subsequent skin grafts healed transiently, until dystrophic pagetoid bone continued to extrude, causing reulceration. The patient has since adopted a program of chronic maintenance care and she remains healthy. Key points: Integra can be used in situ as a reactor or incubator to engineer a new tissue with impregnated cells not derived from the substrate wound.
|
|
Figure 66 Case study I8 (a, top left) This is the radiation ulcer of the scalp, just after
debridement, prior to placing Integra. The Integra was impregnated with
a paste of wound activated cells harvested from a donor wound. (b, top right) The matrix at 2 weeks. Some small unmacerated
yellow fat lobules are present from the original seeding. Scattered
through the matrix, especially center, right, and top, are multiple blooms of
pink regenerative tissue. (c, middle left) The matrix 4 weeks later,
fully regenerated, just prior to peeling the silicone and placing another
layer of Integra. (d, middle right) The second piece of Integra completely
regenerated and ready for skin grafts. (e, bottom left) The skin grafts appear normal at 2 weeks. (f, bottom right) Five months later, pagetoid bone is starting to extrude through the reconstruction, but most of the reconstructed skin is still present. The matrix presumably was populated in part by cells derived from the wound, blood borne or locally resident, but the images suggest that it was mainly the cell transplants which generated the neodermis. |
END • END
• END
Managing Complex and Pathological Wounds
with Integra®
A Gallery of Cases
Marc E. Gottlieb, MD, FACS