|
|
|
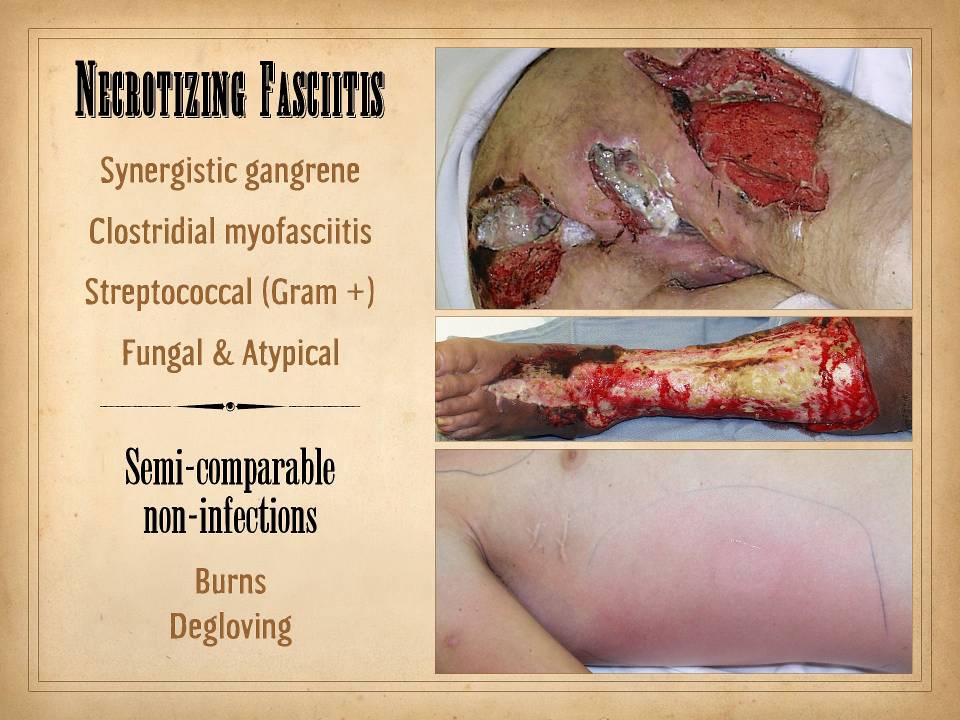
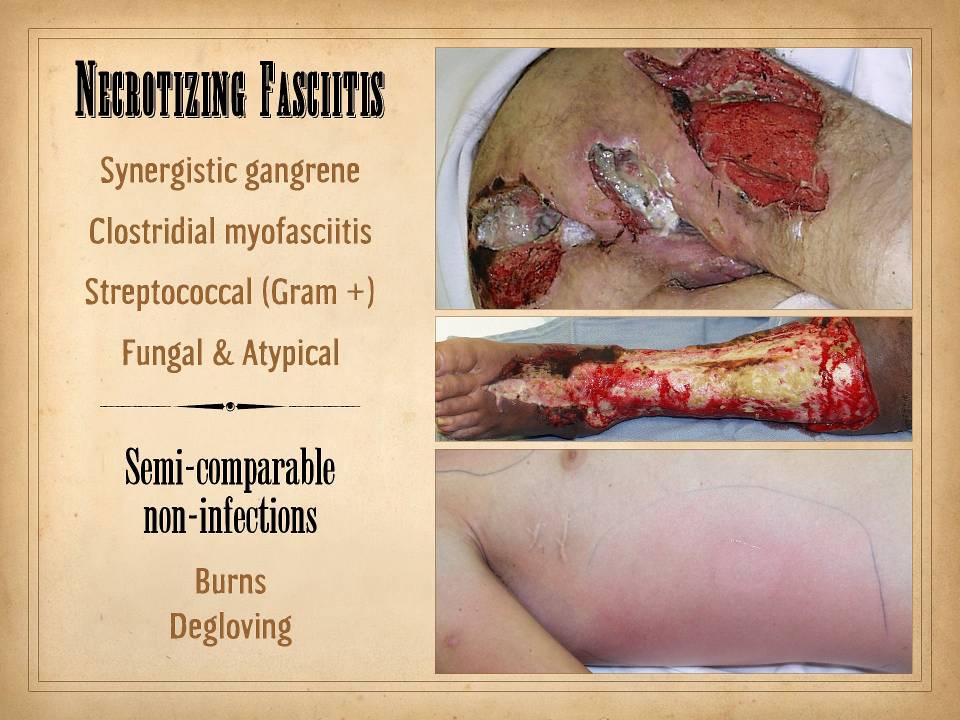
SLIDE SUMMARY: Necrotizing fasciitis is characterized by
pannicular and fascial necrosis.
However, it can be caused by a variety of infectious agents, and each
syndrome has some distinctive pathological and therapeutic features. If not otherwise specified, “necrotizing
fasciitis” tends to imply that due to streptococcus. Surgical treatment by complete excision and
drainage is mandatory. Later
reconstruction depends on principles related to large wounds of any cause.
|
|
------------------------------------------------------------------------------------------------------------------------------------
|
|
|
|
Numerous papers and
book chapters exist to educate you on the basic biology and clinical science
behind these infections. This
presentation will focus on the clinical arts of managing these problems for
good results: for acute life-saving treatment and for long term
function-restoring management.
|
|
|
|
Necrotizing
fasciitis can mean any of several forms of severe, rapidly progressive and
lethal (if untreated) infections. Much
of the drama and public attention to “necrotizing fasciitis” goes to classic
Group A streptococcal panniculitis.
The terminology is not important.
Understanding the behavior of these infections, is important: the
generic implications for life and death and urgent thorough treatment, but
also the relative differences and nuances of care that arise from the types
of organisms that are responsible.
|
|
|
|
All necrotizing
fasciitides have in common that the infection causes infarction and
destruction of tissue, far in excess of the normal injury that occurs from
reactive inflammation. As with most
inflammatory soft tissue pathologies, the primary target or susceptible
tissues are the subcutaneous adipose fascias.
Rapid extension of the disease, tangentially through the fascias, is
the norm. Skin necrosis is typically a
secondary event, due to loss of the trans-pannicular perforators which
provide blood supply to the skin, or due to toxic chemical injury from the
organism (depending on the type of infection). Muscular fascias are likewise more
resistant, and muscles underneath, or viscera, can be involved by extension
(or they can be a primary target for Clostridia).
|
|
|
|
When the disease is
active and rapidly spreading, gross pathology can be divided into several
zones which have implications for surgical treatment (see Slide 7).
|
|
|
|
General classes of
rapidly progressive infectious panniculitis, or toxic necrotizing fasciitis
include these:
|
|
|
|
Synergistic
gangrene: This is the most common type
in daily medical practice. It is
usually due to a mixed flora of pyogenic enteric organisms, typically aerobes
and anaerobes, which create synergistic microenvironments which facilitate
each others growth and metabolism.
Being due to enteric flora, these infections are most prevalent in
abdominal and pelvic related problems, including bowel perforations,
complicated genitourinary infections, enteric contamination of skin and
musculoskeletal laceration or ulceration, perianal or perirectal abscesses,
and so on - including the classic Fournier’s gangrene. Pathologically, there is progressive
suppuration and abscess formation in the adipose panniculus, working its way
into various fascial planes, and sometimes killing muscle. Patients can be extremely ill from general
inflammatory effects and from endotoxins and others toxins. These patients can be gravely ill, and
prompt drainage and debridement are mandatory. However, the biology of these infections
are distinctly different than the “necrotizing fasciitis” of streptococcal
infamy. These infections are due to
organisms which are individually fairly benign, the stuff of everyday GI and
GU infections. It is in the synergy of
mixed flora that they become more destructive. There is a bit of latitude in the surgical
treatment: there is no lesser sense of
urgency, and delays in care ARE NOT excusable, and thorough debridement
remains the goal - BUT - if the exigencies of the illness and logistics of a
trip to the OR are hampered in any way, these patients have a bit more leeway
for a simpler drainage and debridement.
For example, if the problem occurred in the groin after a vascular
procedure, and the patient is on potent anti-platelet drugs, these abscesses
can be effectively managed by gross debridement of loose necrosis and pus,
and wide opening of the wound, but without incurring the bleeding of a formal
sharp excision through still viable but highly inflamed and hyperemic
tissues. This will generally arrest
progress of the infection, while maintaining a good risk-benefit balance for
the patient. Broad spectrum
antibiotics are obviously mandatory.
|
|
|
|
Clostridial
myofasciitis - Aka “gas gangrene”, is often the result of ranch and soil
injuries, or enteric injuries. This is
a serious fulminant disease which requires a serious expedited surgical
response. Muscles as well as fascias
are targets. Exotoxins have lytic
necrotizing effects on the infected tissues, but they also have disseminated
intercurrent toxicities for other organs.
No delays in management can be tolerated.
|
|
|
|
Streptococcal
fasciitis. This is what people really
mean when they talk about the classic N.F.
Strep species other than in Group A, and staphylococcal species can
all cause the same syndrome.
Incidental other organisms can cause the same thing, including
unexpected oddballs such as salmonella.
However, it is the exotoxins in Group A strep which are particularly
pernicious and prone to rapid spreading and “streptococcal toxic shock
syndrome” (STSS) with intercurrent organ failure. It can start off a bit more insidiously
than some of the other types of fasciitis, but when the diagnosis is made,
the imperative for rapid surgery is the same as for gas gangrene. These types of fasciitis can have
distinctive findings, including:
non-odorous (as opposed to synergistic or enteric gangrene); fascial
necrosis and suppuration are often not lytic and cavitary (as is the case for
enteric abscesses); severe watery edema, which is a survival and
proliferative advantage for the organisms;
scarlet color. Complete
thorough excision is required. See
Slide 7 for more details.
|
|
|
|
Atypical
infections. These are due to fungus,
mycobacteria, actinomycetes, and such atypical non-bacterial pathogens. They tend to be “slow” infections - think
TB versus pneumonia or a post-pneumonic abscess - but once vessels start to
occlude and tissues infarct, the destruction can seem to occur quickly. Typically, a relatively slow granulomatous
inflammation was cooking in the fascias prior to severe skin
involvement. Mucormycosis is
distinctive in that vascular occlusion rather than inflammation or
exotoxicity is the cause of problems.
These patients typically have a more insidious and seemingly less
urgent onset, but the implications for curative surgery and reconstruction
are the same.
|
|
|
|
As discussed in
later slides, surgical excision is mandatory, and the sooner the better, with
Clostridial and Streptococcal N.F. having the most immediacy for
surgery. However, the nature of the
required surgery is the same for all such patients with any of these
diseases. Surgery is required for
three components of the problem:
|
|
1 - GET RID OF THE
DISEASE, by as thorough and complete wound excision or debridement as
possible.
|
|
2 - PATCH UP THE
RESULTING WOUNDS, by the the usual arts of plastic surgery, whenever wound
conditions and patient conditions permit.
|
|
3 - RECONSTRUCT LATE
SEQUELAE such as scar contractures, or amputation management, etc.
|
|
|
|
The surgery is
analogous to the surgery needed for burns, deglovings, and any large or acute
wound. Burns and trauma do not have
the same type of illness, and acute and critical patient management are
different than N.F. in many ways. But,
the surgery of cleaning up the mess, preparing the wounds for closure, then
patching them up, then restoring function - that is what core plastic surgery
is all about. Large wounds, small
wounds - it doesn’t make a difference - the surgical principles and methods
arte the same for all of these conditions.
|
|
|
|
------------------------------------------------------------------------------------------------------------------------------------
|
|
TOP - A young
derelict paraplegic patient with long standing pressure sores. Synergistic fasciitis - Fournier’s gangrene
- is a very infrequent complication of ordinary ischial pressure ulcers, and
in fact, it was not the problem here.
Rather the patient developed pressure necrosis of the anus, leading to
ischiorectal infection, which then spread rapidly, involving tissues
throughout the buttock, pelvis, and thigh, including other pressure
bursas. The image here is a couple of
weeks after debridement and wound care, ready to begin closure.
|
|
|
|
CENTER - A patient
with severe rheumatoid and multi-drug immunosuppression developed fairly
rapid skin necrosis, leg ulceration, and febrile toxicity. While rheumatoid panniculitis notoriously
causes extensive ulceration of the leg, that process is relatively slow and
indolent, and does not involve the muscular proximal leg. Biopsies and cultures showed aspergillus.
|
|
|
|
BOTTOM - This is a
19 year old man who developed fevers and malaise after a minor skin
scrape. This was followed by rapid
erythroderma, edema, pain, and progressive toxicity. This is the quintessential Group A Strep
N.F.
|
|
|
|
|