|
Marc E. Gottlieb, MD, FACS A Professional Corporation |
PLASTIC & RECONSTRUCTIVE SURGERY Board Certification ŸŸŸ ŸŸŸ ŸŸŸ Plastic Surgery ŸŸŸ Hand Surgery ŸŸŸ General Surgery |
|
|
Specializing in the treatment, reconstruction, and management of
Acute and chronic wounds Ÿ Diseases and defects of the soft tissues Ÿ Injuries, diseases, and defects of the hand and extremities Ÿ Defects of the head and
trunk |
|
Office: |
|
INTEGRA AND THE MEDICARE PATIENT
Marc E.Gottlieb, MD, FACS
Phoenix, Arizona
July 11, 2003
Slide 1
Integra Artificial
Skin is an implant that is used for closing wounds and reconstructing missing
skin. Originally developed for treating
burns, this material has been of exceptional value in treating many types of
acute wounds and chronic ulcers. This
presentation is a brief look at the kinds of patients and problems that Integra
is used to treat, with the emphasis on elderly Medicare patients.
Slide 2
The following are the
main points to be made.
- Integra is an implant, applied to the
surface, which has two main functions:
in the short term, it is an effective artificial skin, serving as a high
quality skin substitute useful for problems like burns, fasciitis, degloving
injuries, and any other wound, large or small, which would benefit from
biological “closure” without having to take additional skin from the patient’s
own body. It has the second effect of
actually regenerating healthy new tissue, transforming in the process from an
empty sponge to a lamina of autogenous dermis.
- It is unique. There is no comparable
product. Without it, surgical practices
for wounds and burns would have to revert to principles and standards of ten
years ago.
- Integra is nominally simple to use: debride the wound and lay the material
on. It creates tissue and heals wounds
without using any autogenous donor material.
It’s unique properties allow it to solve difficult problems easily. For example, it’s spongy nature allows
regenerating tissue to advance tangentially through the material, allowing new
tissue to form over bones, joints, tendons, and hardware, situations which
classically need to be covered with flaps.
These properties mean that good results are achieved with low resource
utilization and extremely low risk to the patient.
- It’s abilities to heal certain wounds and
salvage complex situations with low risk and morbidity mean that Integra saves
lives (fasciitis, burns, etc.), saves limbs (for the many problems such as
diabetic or arterial foot ulcers which often result in leg amputation), and
thereby saves the lifestyle and livelihood of many patients.
- By simplifying care, by avoiding complex
surgery, by diverting care out of the hospitals and into outpatient venues, by
avoiding secondary morbidity and treatment failures, Integra minimizes the
direct expenses of care compared to conventional approaches to treatment of
many wounds.
- It’s simplicity of use and the nature of the
required pre-operative and post-operative care mean that, for most patients,
all of the required care can be managed through outpatient venues - office or
clinic, and outpatient surgery centers.
- For many problem wounds, Integra achieves
good results when nothing else will, and it does so with minimum risk and
expense compared to conventional care.
Integra is a young product, not yet widely adopted, but penetrating the
market further as it is appearing in meetings, journal papers, and
textbooks. It’s superiority to
conventional care for certain problems means that it is itself becoming the
standard of care among those who use it.
NOTES on the
Technical Use of Integra
This is a summary of
Integra for those not familiar with it.
- The material was first developed in Boston
beginning about 30 years ago. A
collaboration between Dr. Burke, a burn surgeon, and Dr. Yannas, a chemical
engineer, the original intent of the material was to be a skin substitute for
severe burns. Integra was FDA approved
for market in 1996.
- The main component of Integra is a spongy
material made of type 1 collagen (from bovine achilles tendon) and
chondroitin-6-sulfate (from shark cartilage).
The collagen gives structural stability.
The chondroitin is a glycosaminoglycan (gag) that flags cells that it is
a normal embryonic constituent of the body.
The sponge has been deliberately engineered to have a reticulum size
comparable to the collagen in normal human dermis, another essential property
that tells host cells to regenerate tissue rather than make scar. The Integra sponge is prepared in thin sheets
(approx 1mm thick), and then overlayered with a thin sheet of silicone rubber
which acts as a protective barrier, an artificial epidermis. It is sterilely packaged and can be stocked
in unlimited quantity, available for use whenever needed.
- Indications for Integra, and the rationale
for selecting it versus other methods of closure will be illustrated in the
subsequent case studies. While there are
a number of indications for using Integra, the details of its use are
comparable regardless of diagnosis.
Surgeons have certain criteria by which they judge a wound ready to be
closed (be it skin grafts, flaps, Integra, or anything else). All wounds, patients, and their physicians
must practice some basic care to get a wound ready for surgical closure. The essentials of preparatory debridement,
wound hygiene, and control of edema and inflammation are essential to any wound
closure, including Integra. These
activities are practiced until the wound is ready for closure.
- Once the wound has been prepared, closure of
the wound with Integra is done in the operating room. The existing wound, all exposed surfaces, are
excised. The Integra is placed on the
wound and secured with sutures or staples.
Protective dressings are applied to maintain firm contact between the
material and the underlying wound.
- Dressings are typically changed at one week
intervals, in office or clinic. Because
the outer silicone layer is transparent, the regeneration process, the
formation of a new dermis in the underlying matrix, can be readily observed. The material is “regenerated”, i.e. ingrown
with healthy new tissue, on average at about 4 weeks (typical range 3 - 8
weeks). Whenever the dermal regeneration
is complete, a second procedure is done to peel off the silicone and place skin
grafts, thin autogenous grafts using epidermis only, thereby completing the
reconstruction.
- Follow-up dressings and other basic care are
required for a few weeks until fully healed, all managed as a an outpatient.
The physical,
chemical, and biological properties of Integra which confer its dependability
and high quality results are too numerous and technical to detail here, but a
couple of examples will give some insight into why Integra is superior to other
conventional options for the care and closure of certain wounds:
- Integra is comparable in some ways to using
cadaver skin, pigskin, and even the patient’s own skin as a “biological
dressing” to help control a wound and provide temporary skin closure. Unlike these other materials, Integra is not
alive to begin with, so it does not die nor degrade as those other materials
do. Therefore, it need not be replaced
every few days, and autogenous grafts need not be wasted from the patient
himself. Instead, Integra can be placed
once only. As a true artificial skin, it
will protect the wound as long as it needs protection, and then it does double
duty as the agent of autogenous skin regeneration.
- The ability of the material to conduct tissue
growth tangentially means that new
tissue can form over bone, tendon, internal organs, even open joints and
alloplastic hardware, eliminating the need for autogenous flaps.
- The normal response to injury is an
integrated process known as inflammation-wound repair. The moment that Integra is placed on a wound,
inflammation ceases and the normal repair process never occurs. This means that progressive wound damage due
to inflammation ceases, making Integra a valuable and dependable choice to
close wounds subject to “pathergy” (an unanticipated adverse reaction of
tissues to trauma, resulting in necrosis, ulceration, dehiscence, etc.,
typically in cases of severe vascular insufficiency and abnormal immunopathic
disease). Integra instead regenerates by
a process of embryonic histogenesis., leading to healthy new tissues that seem
resistant to the effects of the diseases that caused the original ulcers.
Slide 3
To examine the role
of Integra in Medicare patients, this presentation will focus on a few of the
common classes and causes of chronic wounds and ulceration. The first class is arterial diseases. There are various causes of vasculopathy and
arterial insufficiency. The most common
by far is atherosclerosis, a very common and high profile problem in the
Medicare population. Arterial
insufficiency due to atherosclerosis can be of variable severity and clinical
consequence. Once necrosis and
ulceration develop on the foot or leg, the natural history of the problem is
one of progressive necrosis, ulceration, infection, and gangrene, leading to
loss of limb or life.
The general plan of
care for ulcerated vascular patients is to first provide some basic protective
wound care and then assess the severity and vascular anatomy of the
problem. Revascularization of the
extremity is of paramount importance (by surgical bypass or endovascular
procedures), but it is not always technically possible. Pharmacological agents and hyperbaric oxygen
are helpful adjuncts to care for some patients.
Once these preliminary components of care and correction are in place,
then the wounds themselves must be managed.
These wounds are typically slow to heal.
If surgery is contemplated, there is an important caveat: for any given ulcer or skin defect and the
set of conventional wound closure methods that might close that defect, these
choices are much riskier than in any other patient (e.g. a comparable trauma
wound in a young healthy patient). The
problem is twofold, (1) the arterial insufficiency inhibits healing, making it
harder for flaps to heal or harder for a skin graft to even stay alive on the
wound, and (2) any additional incisions or donor sites, such as for creating a
flap, are subject to the risk of further necrosis and ulceration. This is why conventional surgery has always
opted for amputation: remove the
diseased part at a level high enough to avoid the effects of the vascular
insufficiency make sure that the amputation incision heals.
(NOTE: all of the cases presented here are elderly
patients who were either covered by Medicare, or else presumed to be covered by
Medicare or at least eligible for Medicare because of their age.)
Slide 4

This patient is a
paradigm example of the patient with atherosclerosis, arterial insufficiency,
foot necrosis, and expected leg amputation.
The patient was placed on basic temporizing protective wound care (good
hygiene and silver sulfadiazine), and vascular evaluation was done, leading to
a femoral-tibial bypass. The wound
healing process began to appear.
However, extensive exposure of bone and joint would normally have lead
to below-knee amputation, even after the revascularization (top left photo).
At this point, a
précis of contemporary surgical history is worthwhile. Vascular evaluation leading to vascular
reconstruction is the standard of care for managing peripheral arterial disease
and its complications. However, it is
still quite common for patients such as this one to be seen first by an
orthopedic surgeon, and to have a hasty and indiscriminate leg amputation,
without any vascular surgery input. In
bygone eras when wound care concepts were abysmal, there were no antibiotics,
and the surgery of atherosclerosis was a fantasy, pre-emptive amputation was
the proper thing to do. The foundation
concepts and tools which permit “limb salvage” began to appear after World War
II. By the mid 1970’s, vascular surgeons
had firmly established what is still the nominal standard of care for ischemic
leg ulceration: vascular assessment and revascularization. However, for most vascular surgeons, their
concept of limb salvage means that either a simple wound heals after
revascularization, or a complex wound (exposed bones and joints, etc) can then
be safely amputated, knowing that the amputation will heal reliably after the
revascularization. The idea that the
complex open foot itself could be treated and salvaged remains an odd concept
to most surgeons. Rightly so, because
all of the modern arts and sciences of complex wound closure - aka plastic
surgery, current standards in place by the mid 1980’s - are confounded by
peripheral arterial disease. The reasons
are that it is hard enough to find a dependable flap on the foot, arterial
diseases make the risk of flap complications very high, the chances of wound
complications are high with or without flaps, and a free flap (used when there
are no nearby flaps) cannot be used because the vascular disease prevents
revascularization of the flap.
So, the current
standards of care, pioneered by vascular surgeons in the 1960’s are still the
common standards of care for arterial leg and foot ulcers: revascularize the limb, let the simple ulcers
heal, and amputate the complex problems, knowing that the amputation will heal
after revascularization. Complex foot
salvage, i.e. closing ulcerated bones and joints and so on, cannot easily be
done, so don’t bother to try. However,
times change and advances are made, and Integra is one of the tools which has
made complex foot salvage a successful reality.
Preliminary revascularization is still vital, but now, the damaged foot
itself can be closed, with low morbidity, few risks and complications, low
resource utilization, and good likelihood of success.
In this particular
case, after revascularization, the foot had a final debridement, and Integra
was used to close all of the open structures of the foot. As the material regenerated (upper right
photo), skin grafts were placed (photos left center and below show the
intermediate stages of recovery), leading to a healed foot (bottom right).
Slide 5

This patient was
cared for along the “pre-vascular surgery” philosophy of care. An orthopedic surgeon amputated toes for
complications of vascular disease, without checking circulation nor getting a
vascular surgery consult. the amputation
failed, leading to foot necrosis, leading to below knee amputation, which in
turn failed leading to above knee amputation.
This too failed. The orthopedic
surgeon then wanted to do a hip disarticulation. Contra-indicated for many reasons, that too
would have failed because of the high (aorto-iliac) level of vascular
occlusion. At this point consultation
was placed. After some initial good
topical wound care, the thigh was healed by excision of the defect, Integra,
and two weeks of hyperbaric oxygen support.
Going forward from the point of starting good wound care and skin
reconstruction with Integra, he was cared for as an outpatient. There were no complications, no treatment
failures, no unanticipated therapy. Even
hyperbaric oxygen was used for a deliberate short period of time in support of
the acute post-operative wound. The key
ingredient was the Integra, which by its ability to control inflammation and
inflammatory tissue injury, allowed this very high risk wound to heal without
further necrosis. The net result of a
successful and uncomplicated treatment plan was not only a healed patient, but
a minimum of resource utilization by eliminating complications, failed care,
and redo surgery.
Arterial ulcers and
their care share much with ulcers of any cause, but they have some notable
features. It is the only class of
diseases which predictably and unavoidably leads to leg amputation (diabetic
ulcers are the other problem which predictably lead to amputation, but many of
these amputations are avoidable even with good conventional care). Amputation leads to loss of function and
independence, and for many elderly patients starts a downward trend of
increasing morbidity and dependence leading to death. Failed amputations and wound care lead to
multiple unplanned operations. Vascular
disease implies significant co-morbidities, and these patients are at risk for
numerous complications and prolonged care after their in-patient amputations
and related operations.
Integra applied to
arterial ulcers closes complex wounds, thereby saving limbs and associated
function. Integra avoids the
conventional pathergy and tissue injury complications of surgery, and it can
correct these problems when such complications have already occurred. It’s use tends towards a single successful
planned reconstruction (two stages, Integra then skin graft), rather than a
series of unplanned cleanup procedures as each fails. By minimizing the operative and anesthetic
risk to the patient, and by keeping the care within outpatient venues,
secondary complications and accrued expense are minimized or eliminated.
Slide 6
“Venous disease”,
meaning venous hypertension and insufficiency, venous vasculitis, venous
reflux, and venous stasis dermatitis, is the most common cause of chronic leg
ulceration. This problem never leads to
limb necrosis and amputation, but it does cause significant interference in
normal activities, lifestyle, and economic productivity. Recurrent episodes of stasis dermatitis are
often erroneously misdiagnosed as infection, leading to numerous
hospitalizations. Large sums of money
are wasted on inept “wound care”.
Misguided and premature attempts to “heal” the wound with skin grafts
usually fail. With good care, these
problems can be avoided. “Good care”
generally means good wound hygiene, and the control of venous hypertension and
leg edema by the use of compression bandages or stockings, exercise, and habits
of leg elevation. With good care, most
venous ulcers heal. These forms of good
care have low resource utilization, and as maintenance or preventive care,
ulcer recurrence can be avoided. Used as
palliative care on older or more refractory ulcers, the open wounds can be kept
healthy and need not interfere with the rest of a patient’s normal daily
activities. For some patients, ulcer
excision and skin reconstruction with skin grafts is a suitable and
conventional treatment strategy, but recurrent ulceration through the old skin
grafts is a common problem.
Venous disease and
venous ulcers affect people of all ages.
It is not a disease of aging, but in elderly patients who have had
venous leg ulcers for many years, the ulcers become progressively harder to
treat, due to the chronic accumulation of scar tissue and iron-laden debris
within the tissues. Also, as people age,
the essentials of good treatment for venous ulcers (hygiene, compression,
elevation, etc.) become harder for patients to administer to themselves. Age, infirmity, arthritis of back, hips, and
hands, obesity, visual impairments, tremors, senile skin fragility, and other
factors mean that these treatments, which are simple and low tech in principle,
become impossible to manage when people cannot bend over to wash their feet,
wrap on dressings, and apply stiff elastic stockings. Thus, venous ulcers become more problematic
in the elderly Medicare population, incurring more failed care, more morbidity,
and more expense.
Slide 7

These are two
examples of typical chronic venous ulceration in elderly patients. On the left, this 77 year old man has typical
chronic stasis changes of the medial leg and ankle. A dead piece of recent skin graft is in the
middle, a well-intended but misguided operation doomed to fail because the
dermatitis, debris, and inflammation have not been controlled. After some basic wound and skin care, and
control of edema and venous hypertension, the leg was relatively healthy, and
the wound repair process proliferated.
For many patients, the ankle would have healed on its own (by the
natural process of wound contraction and epithelialization). In this case, the longevity of the disease
and ulcer meant that wound contraction could not overcome the non-compliant
dense surrounding scar. Therefore, wound
excision and skin reconstruction were indicated. Simple skin grafts would have been perfectly
reasonable, but experience has taught that an Integra reconstruction is more
likely to be healthy, less prone to re-ulceration, over long intervals compared
to conventional skin grafts. The bottom
picture shows a healed stable ankle after Integra. All care was as an outpatient.
On the right, this 86
year old woman has a similar history.
The difference is that the longevity and severity of the ulcer have
caused perforation into the ankle capsule and various major tendons. According to the conventions of plastic
surgery, this situation requires coverage with a flap of some sort, not just a
skin graft. With Integra, the issue is
moot, because Integra will work in many of the situations where flaps are
traditionally used, in this case to cover open joint and tendon. After many years of ulceration, the ankle is
healed and stable after Integra. Care
was rendered as an outpatient.
Slide 8

This 88 year old
woman has also had Integra to close chronic venous ulcers of both legs. Note the erythema, edema, and incipient
ulceration of the medial right leg. This
is a flare-up of acute stasis dermatitis.
The acute pathology affects the native skin and subcutaneous fascias,
but not the Integra reconstructed skin elsewhere on the right leg and left
legs.
With venous disease
and ulceration, patient histories are marked by multiple failed operations and
non-operative care. Because venous
problems rarely cause any life-and-limb threatening systemic morbidity, their
disease persists, despite patients and their doctors, for many years. Therefore, the net accumulation of failed
care and wasted resources and expenses becomes very high for some
patients. While patients do not die nor
lose limbs from venous disease, symptoms, expense, and interference with
lifestyle and vocational productivity can become major problems.
Integra typically
repairs these patients when all else has failed. The predictable and dependable course of an
Integra reconstruction means that complications, failures, prolonged care, and
redo surgery are avoided. Stable durable
results mean that patients can return to lifestyle and vocational competence
with only minor intrusions from some some basic daily care to control venous
reflux or hypertension. The regenerated
Integra seems to be relatively resistant to recurrent pathology. Effective and successful planned care, as
opposed to failures, complications, and unplanned redo care, mean that costs
are minimized over the lifetime of each ulcer and of the patient as a
whole. The care is made even more
economical by remaining in outpatient venues.
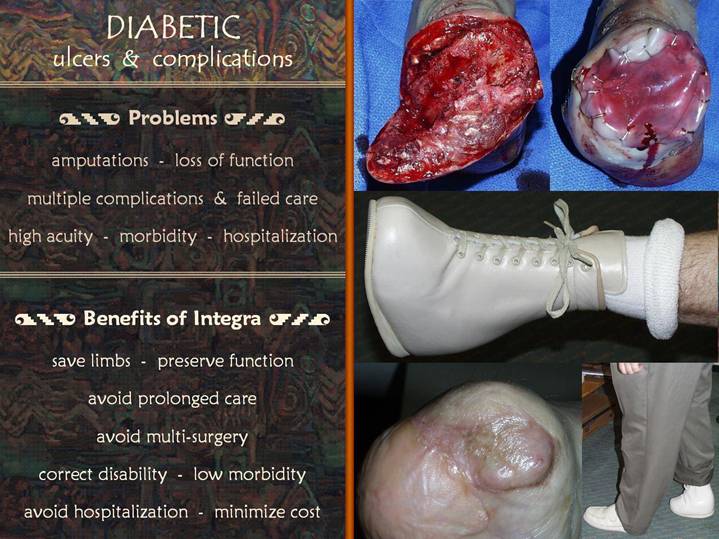
Slide 9

Diabetic ulcers are a
thorny problem, generally perceived as difficult to treat and associated with a
high rate of leg amputation. The
“diabetic ulcer” is not a distinctive form of diabetic pathology, but rather a
syndrome of biomechanical and vascular disorders which collude to create
pressure ulcers of the foot. The causes
of the diabetic foot include: (1)
diabetic peripheral neuropathy, which impairs feeling, so that patients do not
know injury is occurring, and which cause abnormal foot mechanics by paresis of
the intrinsic muscles of the foot (similar “neuropathic ulcers” occur in
conjunction with any form of advanced peripheral neuropathy); (2) glycosylation of tendons and other
structures, leading to abnormal foot mechanics via ligaments and extrinsic
tendons; (3) accelerated
atherosclerosis, leading to the same problems that plague any patient with
arterial insufficiency. The problems
start as indolent occult plantar pressure ulcers, usually unnoticed by the
insensate patient. Persistent and
neglected ulcers are prone to progressive joint destruction, then septic
osteitis, arthritis, and tenovaginitis (tendon sheath infections).
Diabetes and the
diabetic foot are not exclusive to the elderly population, but many of them are
Medicare patients, due to age or disability.
Associated peripheral vascular disease compounds the severity and
recalcitrance of the foot problems.
Amputations occur commonly, sometimes appropriately so (severe life threatening
infections, uncorrectable severe vascular disease, and unreconstructable bone
and joint degeneration causing an unstable ankle or midfoot). Amputations often occur inappropriately, for
simple benign plantar ulcers that can easily be healed by basic judicious wound
care, but which are not, because amputation is how many surgeons, even today,
have been trained to approach the diabetic foot.
Life threatening
infection and amputation are real risks for diabetic patients, and most
diabetic patients and their doctors are aware of these risks. The reality though is that diabetic foot
problems run a spectrum of severity, from simple to life-and-limb
threatening. Assuming that care is being
prescribed and administered by a knowledgeable physician with expertise in this
problem, all that can accurately be said is that effective care can be simple
and outpatient, or it may be prolonged in the intensive care unit, or anything
in between, and it must be planned individually for each patient. Where Integra fits in this picture is that it
will shift patients in the middle away from the complex, expensive, failed,
morbid, amputation end of the scale toward the simpler, less expensive, more
successful, saved-from-a-major-amputation end of the scale
Slide 10

This patient has
diabetes, vascular disease, end stage dialysis-dependent renal disease, and
related diabetic complications. The
right toes are missing from previous vascular problems. The patient required (appropriately) left leg
amputation after developing septic gangrene from a diabetic plantar ulcer. However, as he recuperated from the left leg
amputation, he was allowed to get a large pressure ulcer of the right
heel. The first urge of his surgeons was
to do a below knee-amputation of the remaining right leg. This was unnecessary.
The problem though is
that the calcaneus projects outward far enough that surrounding skin cannot
contract over it. There is not enough
nearby skin to create a suitable flap, and even if there was, the vascular
disease guarantees that the flap will fail, making problems much worse. A free flap of remote tissue is excluded by
the vascular disease. Simple posterior
calcanectomy and closure with Integra is a simple, effective, and dependable
way to solve the problem, with caveats nor contraindications to its use, and no
risk to the patient. It is all
manageable as an outpatient, as was largely done here. The images show the healed Integra (left
panel), the healed foot in a weight bearing stance (upper middle), and the
insert the patient wraps around his heel so that his foot is stable within a
regular sneaker (upper right). By using
the insert and shoe on the salvaged right foot, and by using his left leg
prosthesis and a walker, the patient has maintained mobility and independence
(lower right), all without any complications, nor failed care, nor
unanticipated expense and revised treatment plans.
Slide 11
The most recognizable
“diabetic foot” problem is the mal perforans ulcer under the metatarsal
heads. While pre-emptive leg amputation
(unnecessary, but unfortunately still practiced by many surgeons) is the late
outcome that all good care works to avoid, amputation of toes and forefoot is
another story. The destruction of the
metatarsal heads means that forefoot amputation may be categorically necessary,
and this is completely acceptable, because it need not result in any
significant disability.
This patient
illustrates the conventional caveat that even salvage- and
reconstruction-minded surgeons must face in this situation. After transtarsal amputation of the forefoot,
the remaining tissues are healthy and suitable for wound closure. However, there is not enough skin to close
the open bones and joints. In principle,
more bone could be removed, recessing the bone far enough behind the skin edges
to allow the skin to close. The problem
though is that this is currently a functionally good amputation, with all major
ankle controlling tendons still attached. Further bone resection would detach
these tendons, making the ankle flail and unstable, unsuitable for walking, and
making a below knee amputation more sensible.
If the bone is to be kept as is, how do you get enough skin to cover
it? Conventional plastic surgery
principles dictate that flaps are needed for this situation, not skin grafts,
but there are no flaps around. Even if
there was an available flap, it would likely fail due to vascular disease, and
free flaps are likewise excluded.
Conventional attempts at salvage and reconstruction will result in risky
operations, complications, progressive disability, and a good chance of still
doing the leg amputation.
Integra obviates
these issues. Its dependable ability to
close bone and joint means that the bone can be kept as is, no flaps need to be
made, and there are no further risks due to additional incisions and vascular disease. The foot healed, the patient got a custom
fitted shoe, and he walks without disability.
Care was mostly outpatient, without complications nor variances from the
expected course of treatment.
With diabetic foot
ulcers, the problems and complications are comparable to those of arterial
insufficiency. Amputations and loss of
function are the feared outcomes. There
are numerous complications and failures of care, and conventional principles of
surgery are confounded by the acuity and morbidity of some of these
patients. Care is typically costly and
incurs significant resource utilization.
Integra is by no
means meant for every diabetic foot problem.
The “diabetic foot” means many things, and many treatment modalities
must be selected for many individual circumstances. However, in those circumstances in which
disease and surgery have resulted in loss of skin, but bones and joints and
other viscera are present and create a functional extremity, Integra can reconstruct
skin and heal the wound in lieu of leg amputation. Because rehabilitation, orthotics, and
disability costs are so much less for foot salvage compared to leg amputation,
the patients get better care, better outcomes, and better lifestyle, all at less
expense, less resource utilization, and less risk with fewer complications and
treatment failures.
Slide 12
Connective tissue
disorders are a major category of leg ulceration. These disorders have various names and
nomenclatures, and they include diseases such as rheumatoid arthritis, lupus,
scleroderma, polymyositis, Sjögren’s syndrome, and the vasculitides. These diseases are part of an extended family
of immunopathies which includes diverse disorders such as pyoderma gangrenosum
and Crohn’s disease of the skin. They
can all cause leg ulcers and wound complications. They will be referred to collectively as
“rheumatoid ulcers” or “immunopathic ulcers”.
Data compiled in the wound clinic in which I work show that these
immunopathic ulcers have the longest length-of-treatment of all of these
various categories of disease and ulceration.
Pain, drainage, odor,
progressive ulceration, and progressive disability are the norm. Unlike arterial diseases, there is no risk of
amputation, and no sudden dramatic conclusion to the problem. Unlike venous ulcers which oftentimes have
relatively benign symptoms which people can live with easily enough, symptoms
in rheumatoid ulcers are usually severe and intrusive. Thus, the ulcers and their symptoms and
disabilities tend to linger and slowly progress over long periods of time,
typically months to years. Treatment of
the ulcers is difficult enough itself, but is further complicated by the
disease: these ulcers do not get better
until underlying disease is controlled, which is a challenge because these
ulcers tend to occur during disease flare-ups, and controlling these diseases
can be notoriously challenging. When
disease is controlled, it is often due to antimetabolite drugs and steroids
which can have their own adverse effects on wound healing.
This is another group
of diseases which can affect almost all age groups. “Rheumatoid ulcers” are difficult to treat in
all age groups, but in the elderly Medicare population, the problem is often
compounded by concurrent arterial or venous disease. As with any of these disorders, infirmities
and disabilities of the elderly can make it difficult for these patients to
care for themselves. For these patients,
prolonged duration of the ulcers means prolonged duration of the the required
care, including home health services, medications and supplies, and related
resources. Integra has been valuable
because it can not only heal these wounds, but the regenerated “juvenile” skin
seems to be durable and resistant to recurrent disease.
Slide 13

The 71 year old woman
at top had long standing rheumatoid arthritis and leg ulceration of nearly 30
years duration. The left and center
photos show aspects of the ulcer, which covered the entire ankle and distal
half of the leg. After excision of skin
and fascias, and skin reconstruction with Integra, the leg is healed.
The 77 year old woman
below had a comparable history. Both
legs were ulcerated continuously ever since her first pregnancy nearly 50 years
ago, and all attempts at care have failed.
Although she has all of the classic symptoms of Sjögren’s syndrome,
nobody ever made the diagnosis. When
seen in consultation, the diagnosis was made, and anti-inflammatory treatment
was started. As the legs and ulcers
improved with introductory therapy, successful surgery could finally be done to
close the wounds. However, the extensive
chronic ulceration will neither support skin grafts nor permit natural
epithelialization. Flaps are an option
in principle, and they are even more indicated to cover the multiple tendons
that will be exposed after excision.
Nevertheless, flaps are both unavailable and risky in this older sicker
patient. Instead, the diseased skin and
fascias can be excised, and the tendons covered and healthy new skin
regenerated with Integra. Photos on the
left show the leg ulcers after some of the introductory care and with Integra
in place. Photos on the right show the
reconstructed healthy skin.
Slide 14

The photos show a 73
year old woman with longstanding leg ulceration. Although it is a very characteristic
rheumatoid ulcer (upper left photo), it was misdiagnosed and mistreated as a
venous ulcer for a long time, and even the rheumatoid arthritis itself was
overlooked. After consultation, the
correct diagnosis was made and anti-rheumatoid treatment was started. The ulcer was then excised, and Integra was
used to reconstruct skin directly over underlying muscles, tendons, and bone
(in lieu of flaps, as would be required by conventional plastic surgery
teachings, upper right photo). The leg
healed completely (lower left photo), all with outpatient care. Approximately two years later, the patient
had a severe flare-up of rheumatoid arthritis, resulting in multiple new ulcers
in the surrounding native skin, but not in the Integra reconstructed skin.
Rheumatoid and
immunopathic ulcers are characterized by misdiagnosis and misdirected
care. However, even with correct
diagnosis and conventional care, there is a high rate of treatment failures,
wasted skin grafts, and pointless hospital admissions. Short term successes are plagued by
predictable recurrences, and the costs of recurrent disease and ineffective
care add up.
With Integra, success
is most likely. As with all of the other
diagnostic categories profiled here, proper diagnosis and proper preliminary
treatment of the wound and disease are essential. Once these preliminary activities are
accomplished, some patients will be on a pathway to complete wound closure by
simple topical care in support of natural wound contraction, and some will do
well with the simplest of operations such as a skin graft. But for those in which ulceration is
extensive or long-standing, for those in which the tissues have advanced
sclerosis or residual disease and inflammation, and for those in which bone,
tendon, joint, and other working structures are exposed, Integra succeeds where
all else has failed. It creates healthy
disease-resistant new skin, and it does so with no autogenous donor sites
(except for the final skin grafts) nor any added risk to the patient. All care is manageable as an outpatient, and
resource utilization is minimized compared to conventional forms of ineffective
care.
Slide 15
The foregoing disease
categories are some of the more common forms of chronic ulceration, but there
are many others. No attempt is made here
to further categorize them. The purpose of this last section is simply to
show that there are many forms of chronic ulceration in elderly and disabled
Medicare patients, and Integra has a role in treating many such patients.
Slide 16

On the left is a
woman with end stage renal disease due to hypertension, with tertiary
hyperparathyroidism. This leads to
extensive small vessel arteriosclerosis and subsequent skin ulceration (the
problem of hyperparathyroid arterial calcinosis is today commonly referred to
as “calciphylaxis”, an erroneous use of this term). The ulcers tend to be on the trunk and
thighs, centered over the flanks and hips.
These ulcers are notoriously painful, disabling, and difficult to
treat. The risk of pathergy and surgical
complications is high, and resolving the wounds with topical care alone
typically involves months or years.
Because of Integra’s ability to control pathergy, these lesions can be
excised and closed with Integra, with a rapid resolution of pain, and an
uncomplicated regeneration leading to closed wounds along typical Integra
timelines.
On the right are two
patients with pressure ulceration of the heel and achilles tendon. Comparable to the heel ulcer previously
shown, Integra was able to easily and completely close these wounds which for
many physicians trigger a leg amputation.
Recall that conventional plastic surgery principles dictate using flaps
over structures like this, but flaps are hard enough to find in these areas,
and the associated vascular disease makes flaps risky or impossible. Simply debriding the wounds and laying
Integra over them allows for a benign, uncomplicated, low utilization
resolution of the problem. Most small
heel ulcers heal with topical care only, but when large ulcers have a
protruding calcaneus necessitating bone resection, Integra is categorically
simpler, cheaper, more effective, and an almost risk free way to ensure a
successful outcome.
Slide 17

The center panel is a
chronic ulcer due to a chronic non-union pseudarthrosis of an old malleolar
fracture. Workup failed to reveal any
other diagnosis. While this is a limited
and localized pathology unlike the systemic or diffuse disorders such as
vascular and rheumatoid diseases, nevertheless it caused such persistent
inflammation that all attempts to care for and close the wound failed for
several years. Debridement and
sequestrectomy (removal of the bone fragments) is required, but the persistent
dermatitis created concerns that conventional forms of closure would fail. After the wound was debrided, the ankle joint
was open, necessitating flaps according to conventional principles. Closure with Integra controlled inflammation
(middle photo) and allowed the wound to heal without complication (bottom).
The right panel shows
an ulcer of many years duration in a patient with severe protein S deficiency
(a hypercoagulable disorder leading to recurrent thrombosis and problem wounds;
the patient herself had had multiple venous thrombosis of the leg). This case is similar to the first in that
persistent inflammation was impossible to control, necrosis and ulceration were
impossible to suppress, and wound healing was impossible to induce with any
other customary diligent approach to care.
Wound excision and closure with Integra immediately controlled
inflammation (middle photo), and the reconstructed skin remained healthy and
durable (bottom).
Regardless of
underlying cause or diagnosis, chronic and pathological wounds are all marked
by prolonged morbidity, multiple failed care, surgical and non-operative, and
high expense due to hospitalization and miscellaneous care. Loss of lifestyle and economic productivity
are also significant.
With Integra,
recalcitrant long standing problems can be effectively resolved,even when all
other efforts to close a wound have failed.
Amputations and disabilities are avoided. By resolving the problem expeditiously (along
a typical timeline of Integra regeneration and reconstruction), wasted expenses
and utilization are eliminated. Care is
largely kept out of the hospital.
Slide 18

The place of Integra
in modern wound medicine and surgery must be understood in relationship to
other products. Wound medicine is a
complex subject with many therapeutic options, some effective and well studied,
and some persistent hokums and nostrums held over from the patent medicine era
of 100 years ago. Among legitimate
therapies, each has a mechanism and a meaningful use, but they are not interchangeable. In the world of heart medicine, digoxin,
propranolol, lidocaine, stents, and balloon pumps are not interchangeable
treatments for generic “heart disease”, and the same is true for wounds. Each good wound therapy has a defined
role. There is in fact nothing even
remotely similar to Integra, neither in its manufacture and materials, nor in
its indications and methods of use.
However, administrative simplifications have lumped Integra together
with other products such as Apligraf and Dermagraft under the designation
“bilaminate skin substitute”. This term
is a nominally correct description of Integra, but there is no more similarity
between Integra and these products as there is between any of them and an open
face peanut butter sandwich (also a bilaminate material).
Integra has two
layers. The working spongy layer of
collagen and chondroitin is made from biological materials (biochemicals, not
cells), but it is not alive. The outer
artificial “epidermis” is made of pure synthetic non-biological silicone. On the market since FDA approval in 1996, it
is made by Integra Life Sciences, and managed by Ethicon / Johnson &
Johnson. As discussed here, it’s role is
to reconstruct skin. It is used as a
surgical implant (implanted on the surface), applied in the operating
room. It is typically applied only once,
just as an artificial joint or ocular lens is placed only once (barring
complications).
Apligraf and
Dermagraft are very similar products, direct competitors in the marketplace and
essentially identical tools for the wound doctor. My own experiences are that Apligraf is a
more effective product, and throughout this discussion I will refer only to
Apligraf, with the implicit understanding that for the sake of this discussion,
“Dermagraft” can be used interchangeably with “Apligraf” with regard to
clinical indications and application.
Apligraf and
Dermagraft are LIVING materials. They
are manufactured from donor neonatal foreskins.
Cells are stripped form the original skin, then grown in cell culture
with nutrients and biochemicals. For
Apligraf, new dermis is grown first, then a living epidermis is grown on top of
the dermis. The result is a
“re-engineered” living skin, living in the petri dish in which it was
grown. To be used, a physician must
order it in advance. It is delivered in
an elaborate package which oftentimes includes a battery driven electronic
heater to maintain temperature within the package. Just before sealing and shipping, the package
is charged with precise amounts of oxygen and carbon dioxide to keep the cells
healthy. The culture medium substrate
has a pH color indicator to show whether the material is still viable and
usable. It must be used within about
24-48 hours of delivery. Apligraf is
made by Organogenesis, a small biotech company.
On the market since about 1999, it was managed by Novartis until January
2003, at which time business disputes between the two companies suspended
manufacture and shipping of the material for 6 months. It is now available again (as of June 2003),
under the sole management of Organogenesis.
When Organogenesis
first made Apligraf, their belief and their marketing campaign were both
organized around the idea that Apligraf was handy-dandy skin graft in a box -
“McSkin”, suitable for use by non-surgeons who wanted to use a skin graft, and
readily available to real surgeons as easily as pulling Kleenex out of a
box. Great for burns and trauma and
whatever - in principle. But this
concept was based on rat models, and rats have different immunological barriers
than people. McSkin works on McRat, but
not on non-veterinary patients. Every
clinician and human biologist knows this - people reject allograft skin. Every physician who follows this was
perplexed about how Organogenesis got FDA approval for the product. Most surgeons who followed these things tried
Apligraf once or twice, realized it didn’t work, just as they expected, and
lost interest in the product, including me.
As a skin graft, it is a non-product.
But it turned out that in the right circumstances, Apligraf was doing
something wonderfully good for chronic pathological wounds. It took a while for practitioners to
understand how to use the product, but it is now an important part of the wound
doctor’s toolbox. Simply put, Apligraf
acts like a pharmaceutical, a drug delivered within a living material, that
stimulates wound healing in recalcitrant or retarded wounds. Somehow, these juvenile cells confer
something beneficial to the problem wound, stimulating a healthier and more
active wound repair process. Novartis
later retrenched their position on “skin in a box”, and at all their later
symposia, they were very forthright, forthcoming, and up front in their
acknowledgement that the “skin in a box” concept was wrong. Their latter research has all been focused on
trying to understand what these neonatal cells are doing to the recipient
wound.
I am personally a fan
of Apligraf. It does wonderful
things. I was also a speaker for
Novartis, involved with their physician education symposia. Meaning - I know something about the product,
I know something from more of an insiders point of view, and I like and support
the product. Therefore, any comparison
of Apligraf and Integra is NOT adversarial nor antagonistic nor mutually
exclusive. As a practitioner who depends
on both of these products, I have a vital interest in seeing that both products
survive and do well, because both have become an integral part of modern wound
practice. Any discussion of the
differences is objective, analytical, and inherently favorable to both
products. What must be realized is that
while both products have a role in wound care, their roles are different, just
as digoxin and stents both have roles, in “heart disease”.
Against this history,
the nature of the original “bilaminate material” designations can be
appreciated. When Integra was developed
and first marketed, It was meant to be a skin substitute for severe burns. It’s ability to induce embryonic new skin
formation and the full panoply of its remarkable uses were not the least bit
anticipated. When Apligraf was first
approved and marketed, within about two years of Integra, it’s intent was to be
a skin graft or skin substitute for any wound.
Its failure as a generic skin graft and its real role as an effective
biopharmaceutical to treat pathological non-healing wounds were not
anticipated. So, both products were
forward thinking bioengineering devices from small biotechnology companies. Both products hit the market nominally as a skin
replacement. Both products were
manufactured with two layers of “stuff” (Integra sponge-silicone, Apligraf
dermis-epidermis). Therefore, both were
seen as bilaminate competitors for the same problems and market segments. Now we see how naive those early days
were. Unfortunately, the original
reimbursement designations for these products, developed in good faith during
the early but conceptually flawed days of these products, are now hampering the
ability to deliver these products for their real uses and benefits to all of
their potential beneficiaries, especially for Integra.
Slide 19
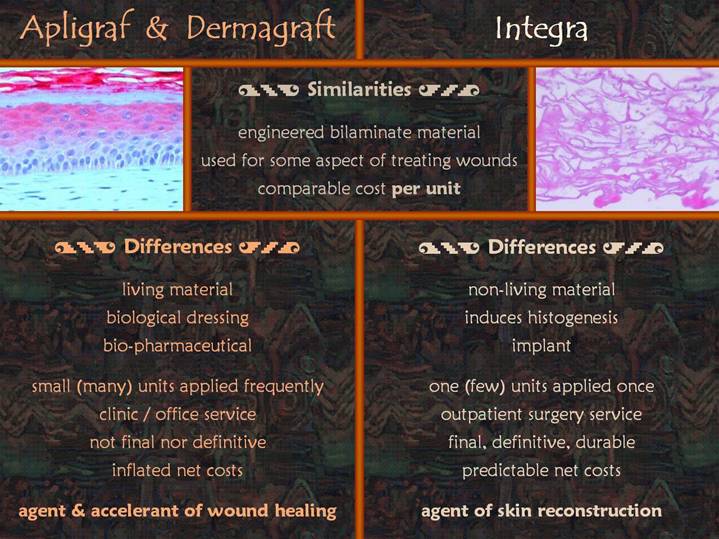
Apligraf (and
Dermagraft) and Integra share some properties.
They are all manufactured. They
are all “bilaminate”. They are all
utilitarian and effective for some aspect of wound care. They all have a comparable cost per packaged
unit (current charges are approximately
$950 for a 44 sq cm (3" diameter) circle of Apligraf: $500 for a comparable size piece of
Dermagraft: $1250 for a 250 sq cm
(4" x 10") sheet of Integra).
The similarities end there.
The left
photomicrograph shows Apligraf. It is
living skin, epidermis on top of dermis.
On the right is Integra, an acellular matrix of biochemicals (the upper
silicone layer is not seen because it usually comes off for histology
processing). This is an emphatic
portrayal of how there is nothing at all structurally similar about these two
products.
Differences between
the products are far more important than the nominal similarities. Apligraf is living. Integra is not living. Apligraf functions as a drug, delivered in a
living vehicle, which stimulates the wound healing process of the recipient
wound. Integra is an implantable scaffold
which suppresses normal wound repair and instead gives host cells a place in
which to regenerate new tissue (histogenesis).
Apligraf does its job, dies, and disappears. Integra becomes incorporated into the host.
As a WOUND
STIMULATING PRODUCT, Apligraf is not the definitive nor final closure of the
wound, but rather a topical treatment that forces the wound to do its own
healing. It is usually applied in office
or clinic, as part of an ordinary outpatient wound visit. It is applied as small standard units (44 sq
cm circles), as many as needed to cover the wound. It’s per-square-centimeter cost (approx
$21.60) makes its use economically prohibitive for large wounds. It is usually used on relatively small
wounds, up to a few centimeters in diameter.
It will often successfully heal a wound after one application, but if it
is effective but incomplete, subsequent “doses” can be applied. The Apligraf treatment paradigm: (1) use it in office or clinic; (2) use small units, as many as needed,
applied as often as needed; (2) wait for
the right time, keeping an eye on the bottom line, because the costs can run up
with large wounds and multiple doses.
As a SKIN
RECONSTRUCTION PRODUCT, an Integra reconstruction is meant to be the final
definitive closure of the wound. It is
used in the operating room. It is
applied in large standard units (typically 250 sq cm, or other stock sizes
suited to the size of the defect). As
many sheets are used as needed to close the defect. The per-square-centimeter cost of $5.00 is
economically sound, especially because it is used only once to build a
successful reconstruction. It’s low cost
makes it economically sound for treating large wounds such as burns and
trauma. The Integra treatment paradigm: (1) it is an implant to be placed in the
operating room; (2) use it to cover any
size defect, large or small, applied once;
(2) intervene to reconstruct early, because early successful use of this
economical product minimizes long term net costs by prompt resolution of the
problem.
Slide 20

While Apligraf and
Integra still carry the designation of “bilaminate skin substitute”, these two
cases illustrate the different therapeutic functions and uses of these two very
important but dissimilar products.
On the left is
patient with a chronic ulcer over the achilles tendon. Skin is ulcerated, but the wound has not
perforated through the skin and subcutaneous fascias into the tendon
itself. Ulcers in this area can be
notoriously hard to heal, predominantly because the biomechanics of this moving
area are adverse to normal wound healing.
On first glance (left end photo), this looks like a normal healthy
healing wound which should be closing by ordinary wound contraction, but it
isn’t. Although managed by good topical
wound care and splints for 4-5 months, the ulcer never varied from this appearance
nor size. If this was a healthy acute
trauma wound, surgical closure would be done with ordinary autogenous skin
grafts because there are no special features of the wound which warrant
anything more elaborate. However,
surgical closure cannot be done because successful surgery depends on a healthy
wound healing process (and if this wound was healing properly, it is small
enough to close without surgery). This
is the perfect place for Apligraf: the
wound appears healthy (no disease, no inflammation, well cared for), and wound
repair is evident but going nowhere. The
seemingly healthy wound needs a friendly “kick in the butt” to start behaving
properly, and this is what the pharmaceutical effect of Apligraf does to a
wound. The middle photo shows the wound
about 5 weeks after placing Apligraf, and the 9 week photo on the right shows
the wound fully healed, a typical time frame for Apligraf to heal a wound. (This 44 year old man is the one patient in
this presentation who is younger and was not a Medicare or Indian Health
Services beneficiary.)
The right hand panel
is another achilles ulcer, but this one cannot be managed by Apligraf. This 65 year old woman has Wegener’s
granulomatosis, a potentially life threatening connective tissue disorder, held
in control by steroids and antimetabolite therapies. Her severe pulmonary complications make her a
poor risk for surgery. The ulcer has
perforated into the achilles tendon.
Basic topical wound care is needed to keep the wound safe and prepared
for surgery, but because the wound cannot heal over the tendon, topical care
alone will not work, including Apligraf.
Conventional principles of plastic surgery demand that this exposed
tendon be closed with a flap. While
there is indeed evidence of wound repair in
the wound, her disease and its therapy make any local flap prone to
complications and a larger wound. A free
flap from a remote location is likewise risky, and even more so in this patient
because of her pulmonary status and the higher risks and potential morbidity in
these long procedures. This is an ideal
Integra case. It will generate new
tissue across the tendon, serving the same function as a flap. It requires no autogenous donor sites. All that is required is a simple wound
debridement and then the application of the Integra. The procedure is very short, outpatient,
inherently not risky, and it can even be done easily with local rather than
general anesthesia. Post-operative care
is basically nothing at all, other than weekly observation to see when the
Integra is regenerated and ready for the completion skin graft. The left photo shows the ulcerated achilles
tendon, the middle photo shows the regenerated Integra at the time of skin
grafting, and the right photo is the healed result.
Integra and Apligraf
share some nominal indications.
According to the provisions of its FDA authorization, Apligraf is
indicated for diabetic and venous wounds.
Integra is indicated for burns.
In actual practice, these products are all used for all of these
conditions. However, these products are
used at different times, under different circumstances, their usage defined by
medical indications rather than regulatory indications. Both are valuable products, essential in
modern wound practice, but their medical indications are as divergent as the
indications for pronestyl and porcine valves in the treatment of heart
disease. These two cases illustrate
those important differences. Apligraf
and Dermagraft are wound healing products, stimulating a refractory,
recalcitrant, retarded or delayed wounds healing process to turn on. Integra is a tissue regeneration product,
creating new tissue to cover structures and close wounds in circumstances where
even a healthy wound healing process needs some surgical help.
Slide 21
It should be evident
at this point that Integra is a valuable product that solves difficult problems
easily and with low risk.
It is important to
emphasize that the product is unique. In
the seven years that this product has been on the market, I have used it nearly
250 times. In a practice that is devoted
to difficult tertiary problems, I have done far more than just 250 operations
in 7 years, and I have seen thousands of patients in outpatient wound
clinics. Integra is not to be used
indiscriminately as a substitute for simple skin grafts, necessary flaps,
topical wound care, wound stimulating therapies, nor anything else. Each therapeutic modality has its
indications, its time and place. When
Integra is indicated, it is often because it is the only thing that will work,
or the patients are too sick for conventional flaps or grafts, or economics and
availability of resources make it desirable, or because the end results are
superior. When it is needed, it is
really needed, and there is simply no substitute.
Slide 22

Here are three final
examples of difficult problems easily solved by Integra.
The hand belongs to a
patient with vascular disease.
Thrombosis or embolism resulted in gangrene (top photo). An important principle of hand surgery is to
try to preserve length and parts, because patients will always find a way to do
something useful with parts of a hand, and the more parts missing, the more
disabled the patient is. Debridement of
necrotic tissue resulted in bare metacarpals without soft tissue coverage
(middle photo). The situation is similar
to the trans-tarsal amputation shown earlier.
Bone could be removed until remaining skin can close over them, but this
would shorten the hand to the wrist - not nearly as useful a hand as if the
metacarpal rays could be preserved.
Flaps would be the conventional approach. Integra has been so good on hands that it is
redefining all of the conventional approaches to hand coverage, but the
discussion is moot in this patient, because vascular disease precludes any kind
of flap. Closure with Integra saves all
salvageable parts of the hand and preserves length and function (bottom photo).
The right upper panel
is a below knee amputation gone bad. As
already illustrated with the previous case of thigh stump necrosis, many
surgeons’ first impulse with a bad amputation is to amputate higher. Below knee amputation at least preserves a
fair bit of function and options for the patient, but above knee amputation is
always a poor choice in elderly patients with vascular disease and related
problems. In cases like this one, some
necrosis of skin and fat need not trigger an above knee amputation. Instead, basic wound care and then Integra
reconstruction over bone and joint salvages an important piece of anatomy and
function. (Top, the open amputation
stump after debridement and preparation.
Middle, the stump soon after placing skin grafts over regenerated Integra. Bottom, the healed stump, with a straight
knee.)
The ankle at the bottom
is has a chronic ulcer due to rheumatoid activity. Refractory to all prior care, it healed
without incident with Integra, all care rendered as an outpatient.
This slide
recapitulates the benefits of Integra.
The issue of outpatient services warrants special discussion. Concepts about fixing wounds, and the tools
and techniques to do so, have made meaningful progress over the past
decade. Along with new tools like
Apligraf and Integra, four “administrative” or logistical conditions have
significantly impacted the way wounds are managed: (1) the advent of dedicated wound clinics,
(2) the ready availability and high quality of home health nursing and related
services, (3) the prevalence of outpatient surgical centers (including general
advances in the safety of anesthesia), and (4), rightly or wrongly, the
pressure by managed care and third party payors to move people out of acute
care facilities. What these conditions
have resulted in is an infrastructure for caring for wound patients that has
its best and most dependable resources outside of the inpatient hospital. Even most of the surgery illustrated by the
cases in this presentation is now done as an outpatient. Many of these are sick, high acuity patients
having procedures which, until beginning in the mid 1980’s, were guaranteed to
be accompanied by an inpatient admission of a week or two.
Keeping patients out
of acute care is a GOOD IDEA.
Predictable expenses for nominal prescribed care are kept much
lower. Irrelevant tests and
consultations are virtually eliminated, and complications and related prolonged
care are kept to a minimum. Patients’
morale and sense of well being are kept higher, and post-operative bed
confinement and resulting disabilities and complications due to deconditioning
are kept very low. These benefits are
especially noticeable in the elderly Medicare population where apriori
diseases, weakness, disabilities, and geropsychiatric problems are significant
predispositions to costly complications and irreversible downturns in
lifestyle. With the looming public
health crisis of an ageing baby-boomer population retiring but living longer,
strengthening outpatient services and models of care is of pre-emptive
importance. For wounds, much of the
outpatient infrastructure of good care is already in place and generally
getting better.
Slide 23

Integra solves tough
problems. It save lives (burns and
fasciitis), limbs, and lifestyles. It
does so with little or no risk to the patient, and it does so largely as an
outpatient. It is an effective and
dependable tool ideally suited to the shifting paradigm of outpatient wound
management. It is a unique product, and
when it is really needed, there is simply no alternative choice. The Medicare population in particular is a
group of patients most likely to get dramatic medical benefits while also
realizing important economic savings by use of this product. Unfortunately, current reimbursement
regulations, established in the early days of these new “bilaminate skin
substitutes” now impede the use of this product in Medicare patients.
In my own practice in
Phoenix, Arizona, Medicare reimbursement policies have had a tangible effect on
using this product in people who need it.
I do most of my surgery, inpatient and outpatient, at St. Joseph’s, a
major urban general hospital and medical center, owned and administered by CHW
(Catholic Healthcare West). I also do
some of my surgery at a free standing outpatient surgical facility. The free standing facility will not allow me
to do outpatient Integra cases, because they are not reimbursed the cost of the
material. Because of managed care
contracts, these patients may have no choice as to venue. For these patients, unless something can be
done to finagle an inpatient admission somewhere, they cannot have
Integra. This has been a de facto
reality for a few patients, and more conventional but less effective modes of
care have had to be used. At St.
Joseph’s, they too do not get reimbursed for the outpatient use of the
material. As a Trauma 1 center in a
Mexican border state, the hospital must assume a lot of debt on unreimbursed
care for undocumented aliens, the problem compounded by the very high managed
care penetration in Arizona, all putting significant financial pressures on the
facility. Nevertheless, they permit me
to do these outpatient Integra cases anyway, because I bring almost all of my
business there, and because they have a charitable mission to take care of all
patients. The special favor that I
receive to do these cases is beneficial to the “system” as a whole by keeping
direct costs of care to a minimum, and it is certainly beneficial to the
patients. However, not all facilities
are likely to be so tolerant or charitable, and in many other communities or
facilities, many potential beneficiaries of this amazing product will not
receive that benefit.
As a physician in
private practice, my own motivation in all of this is simply to do the best I
can do to take care of these patients.
Doing the best often means using Integra, and my interest in preparing
and presenting this lecture is simply to help ensure that the product survive,
flourishes, and is freely available when needed.
Marc E. Gottlieb, MD,
FACS
Phoenix, Arizona
July 11, 2003
END